SPIT! What Your Mouth Microbes Say About Your Health

Total Fitheads
53 Minutes
Episode Transcript
Ali Spagnola00:00
Hey, Fit heads today, we talk with Danny Grannick the CEO and co-founder of Bristle and BRB, I just need to go floss. This was another one of those ones where I'm like, this is terrifying. And tell me more. And I'm like, why haven't we heard about this before? How are you solving this low-hanging fruit and no one's ever brought it up.
Low-hanging fruit. I mean, like he's talking about how this is dealing with your oral health. The microbiome is like up there on things that could make a huge difference in your health and that we're not addressing. And in very easy ways, just as long as you'd be like, know what you're doing targeted with some of this, it seems like there's zero targeting and in oral health care right now, we're all just doing the same thing, going to the dentist, the correct amount of times you think, you know, the number of times you should go to the dentist, you thought wrong.
Keep listening serious fitness for not so serious people. Hey, Danny. Welcome. Hey, thanks for having me. Yeah. So excited to talk to you about mouths. This is dope. People excited. That's it like? Yeah, no one ever. We were just talking before this, like no one's ever. Ooh. I really love my internet service provider.
It's always. Darn Comcast or at, and T to tie it in. No one's ever like, Hey, love, love my dentist. You really like going to get a cleaning. And that's what you think of when you think of oral health. Yeah. Yeah. I think that's I think if you're, if you're fortunate, you don't really think about it. I think most people probably dread thinking about it.
Danny01:54
Brian, in particular, one of our co-founders. Was he a part of like, he had his own problem and that's why that he's making the solution. He's like the, yeah, it was it was a combination we were so like, yeah, the story behind the company was we were at this a pitch contest. We weren't pitching, we were just kind of watching other companies and.
Five companies. I think talking about the gut microbiome and we had both come from the genomics industry. So we're sitting there and we're like, oh my God, how many, how many gut microbiome companies do they have to be? And. Brian had a dental appointment, the doctor say, and he's like the cliche great about oral hygiene.
And it has cavities, like every time he sees the dentist. So he was sitting there just complaining and lamenting about this appointment the next day. And like doesn't work and it still doesn't. Oh yeah. Yeah. Okay. But he also eats like a ton of really just lightened into him on this, but he also just eats a ton of candy.
So I don't think that really helps anything, but he tries and, you know, yeah. Inevitably has cavities and he was kind of lamenting about that. And we were in the midst of talking about this gut microbiome stuff and it really just kind of. That's right in the face that we it was something to look into or we just kind of put two and two together.
Cool. So did you end up pitching at the thing or that being in that environment? Yeah. It was just kind of the combination of like gut microbiome, and then Brian complaining about his upcoming dental appointment. And we were like, huh, like nobody's really, nobody's looked into the oral microbiome. Like we should really take a look.
Okay. Sweet. I love it. Serendipity. So yeah. Can you give the fit heads just to like some background on what Bristle. Yeah. So in case, in case you didn't catch on
So Bristle is I think at our core where we're a biotechnology company. So we, we take saliva and we look at the oral microbiome and that's kind of the makeup of bacteria, fungi and viruses. Live inside of our mouths. You have a gut microbiome, there's a skin microbiome, a bunch of different microbiomes, but we're focused on the one in your mouth.
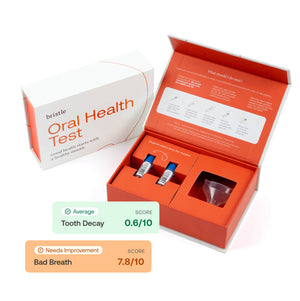
And our, our goal as a company, kind of the short term goal is to use the oral microbiome to help people understand and improve their oral health. So we have a direct to consumer oral microbiome test. You spit in a tube and send it back. And then we analyze those bacteria. Tell you all of the bacteria and fungi and viruses in your mouth and their association to oral health conditions.
So certain bacteria are pathogenic and they're related to things like cavities and gum disease and bad breath, kind of the typical worries that you would have, and the others are really beneficial and can help you fight off disease. And. Maintain good breath and kind of digest foods. And we provide kind of scores and, and help you understand what bacteria you have that contribute to your oral health status.
And then we match that with recommendations around products and diet and hygiene practices to help you get back on track. Interesting. So how many of those dudes are living in my mouth right now about, so let's see. I think there is there's a little over 700 bacteria that have been identified as part of the oral microbiome.
On average, we find between 80 and 120. So it depends on the ratio of pathogenic to non-pathogenic bacteria that you have, and then how those pathogenic bacteria are related to certain conditions. So if you have a lot of the bacteria that are related to, you know, they, they produce acid as a by-product the acid erodes, your enamel that leads to cavities.
You're going to be at risk for cavities and same thing with gum disease and halitosis or bad breath. Interesting. So is there like an ideal profile? That's like the perfect balance of terms? Yeah. I mean, it's something that we're trying to figure out. Like I think, you know, compared to a lot of other parts of biotechnology, like we, you know, when, when sequencing, I think as a technology got relatively commoditized, there's this explosion of data and research, but it's really.
Attributed to, and I think rightfully so, like some of the quote unquote, like worst conditions that we could go after, right? Like cancer. Alzheimer's got microbiome sequencing obviously, and there's been very little research and, and resources devoted to really understanding the oral microbiome and oral health.
So in a lot of ways we're building that database from the ground up. But I think to answer your question. Not having pathogenic bacteria and having a lot of the commensal and beneficial bacteria is the ideal scenario. And you want a good amount of diversity in your oral microbiome. So it's not just, oh, I have, you know, five species of good bacteria.
So I'm okay. You want to have, you know, 80, 90 different kinds of species that all fall into that beneficial bucket and then ideal world. And then. What species make up, you know, somebody oral microbiome versus somebody else's maybe had some differences on oral health, but that's kind of the big goal is you want diversity and you want all of those bacteria to be in that commensal or beneficial bucket.
Okay. What you've seen so far how different is everybody. Mouth, is it like fingerprint or do they sort of fall into buckets or it's? So they're all, they're all different to varying degrees. We see some patterns. So you know, children's oral microbiomes, especially in infancy reflect their mother's oral microbiome pretty well.
And we actually see some similarities and, and partners, right. Because. Swamp and saliva and sharing cups and whatever. Which is interesting because there's also, I mean, there's like a lot of cross-pollination that can occur between the oral microbiomes, but I guess broadly speaking, like there are, I would say patterns of similarities between oral microbiomes, depending on the cohorts that you're looking at.
But like when you get down into the nitty gritty, specific species and ratios everybody's yeah. Hmm. Interesting. See, that's even more of a reason to care, right? Because if you're a mom it's affecting your kid, when I'm going out and ordering a giant blue fishbowl and sharing it with all of my frat friends, I'm affecting them.
Yeah. Putting, putting, everybody at risk. We had some questions like we did a Reddit AMA. Maybe a month or two ago. And there were a lot of questions around, somebody had mentioned, they were like, I, I take antibiotics or whenever I do an antibiotic regimen, all go to a bar and try to find somebody who has like, don't know how they qualify this, but like a good looking mouth.
And they were like, that's.
Make out what then? To like reseed my oral microbiome,
DIY like oral microbiome transplant. Oh, wow. Blocking out. Everyone's.
Huh? Yeah. Interesting. So. Yeah, I guess antibiotics would probably cause problems in your mouth like that too, right? Yeah. I mean, it's the same story that we see with the gut microbiome where antibiotics are, you know, or even pulling it out to over the counter products. Like some mouth washes kills a 99.9, 9% of germs.
Sounds great. Like on the surface. What a lot of people don't realize is that you're wiping out everything. And I think it's, it's kind of akin to the chemotherapy, right? Like, yes, you're getting rid of the bad stuff in your, in your oral microbiome, those pathogenic bacteria, but you're also wiping out all of those commensal and beneficial bacteria that produce.
The pathogenic ones from taking hold. And I think for a lot of people, like as long as you're maintaining good, good hygiene, usually you can mitigate the bad effects, but we've seen a lot of cases of people actually exposing themselves to more pathogenic strains. They create space in the oral cavity for those bacteria to come in and grow, honestly stopped using mouthwash since I've read about that.
So I don't know. I mean, it sounds like you're kind of suggesting that, that, that 99% killing type mouthwash is bad for you. Yeah. I mean, I think, you know, one of the themes that we see in, in oral care is this idea of. Broad spectrum treatment, right? Like we have a bunch of products out in the market. You go to a grocery store and you look at the oral care aisle and there's like 200 different kinds of toothpaste, but they're not actually that different from one another.
Like the ingredients are largely the same and they, I don't know that one has stripes. Yeah, the Stripe one, and obviously it comes out strips. I don't know how they do it.
And There, I would say they're like somewhat beneficial for everybody. Right. But there's this idea. And I think, you know, another thing that personal is we're trying to take a lot of these ideas from molecular biology, things around personalized treatment, precision medicine, and apply them to the oral health space, into the over-the-counter space as well.
It's kind of the same thing. You have broad spectrum treatments that kind of work for everybody, but don't really work for anybody in particular. And it's the same thing with mouthwash, right? Like it generally kind of works for most people, but there is like an inherent risk to wiping out your oral microbiome.
And there's a lot of cases where maybe you do need something that is that harsh. But for your average person, like, there's probably more risk that you're introducing than benefit. And that's what we're trying to kind of sift through in the oral care industry. And then on the toothpaste side, it's the same thing.
There's, you know, fluoride and that's kind of all you see at the grocery store. But there's a lot of other products out there and a lot of ingredients. That have different effects depending on what oral health conditions you're facing and what kind of oral microbiome you have, ah, personalized health care, but for your Val, it was just that it's just that commercial.
I remember that commercial, that old mouthwash commercial, where they like zoom into your gums and there's all these cartoon. Air quotes, germs, the lick and their meat. They have like a mean face on, and then the liquid comes in and they all strengthened and nothing. And I'm like, oh my God, that's in my mouth.
I need, I need that right now. You know? But they bamboozled me well that initially knit blistering was just marketing. Right. They invented halitosis. They made us scared about something that we did. Even care about, and then suddenly Listerine took off. They, I mean, I remember reading about this, how it was just.
Yeah, they made up marketing about how Edna couldn't get a husband because she was beautiful and everything was right. Except she had this halitosis that, and everyone was like, wait, what's that? And now suddenly I week I'll care about halitosis. They did a great job. I mean, I think halitosis is like, literally.
Creek for bad breath or something. And that's not to say, I mean, like halitosis is like a very, obviously it's a very real condition, but they did a fantastic job of marketing like this relatively and effective solution for, for a labeled condition. I think it existed, but existed in a lot more shades of gray than the umbrella term that they kind of like slapped on top of it.
And that's, it's true, like across the dental industry. So the idea of seeing your dentist twice a year originated from an ad, it was a Pepsi dent. Toothpaste company ad from the 1950s. And I I'll I'll dig it up and send it to you guys after this, but literally like a little cartoon that's I can't remember it's some stupid rhyme, but something about going to see your dentist twice a year and using Pepsident every day.
And that was the origination of the twice yearly dental visit. So. Wait, you're telling me as you go by weekly, like once a day, what? Yeah, I mean, just like everything else had pads on the person. There was, there was a really good study done by the NHS. So the European kind of like healthcare system in England and they did a, a really big.
Trial called the interval trial and showed that there was no difference in oral health outcomes. If you stratify for risk for low risk individuals, if they saw a dentist, every, I think it was like three months versus once every two years. So the idea is like, we've kind of been ingrained with this.
Ritual of like going to the dentist and getting these cleanings and, you know, finding out you have a cavity or you don't, and then going back in for your filling and, and the reality is, you know, you can prevent a lot of these conditions just by understanding what your status is and making some small interventions along the way.
And you don't have to go in nearly as much as, as you think you do well. Well, jokester on you because my dentist is my uncle. So I see him all the time.
Yes. Ask him weird mouth questions at dinner all the time for free. This is not the time.
Okay. So then let's talk about some of the things you're suggesting. It sounds like there precision products out there that will work specifically for what I need. Like what, what kind of stuff are you offering the people once you've seen what's going on in there? Yeah, so I think it's, it's like, there's two things that we're trying to solve for it.
There's. Ingredients out there and we have some data about which ingredients are going to be more partial to somebody. So if you. You know, if your score comes back and you've got more bacteria related to gum inflammation than you do tooth decay, there are certain ingredients and certain hygiene practices that we'll recommend depending on like what you do or don't do right now that are going to be more effective than something we would recommend for battling tooth decay.
You know, I think like for everybody out there who might have bad breath, tongue scraping is like one of these. Nobody really talks about it. It, it works wonders. So that would be like a behavioral change that we would recommend. And there's other products out there xylitol is, is kind of this really interesting sugar derivative that, that bacteria.
Consumer they can't process. Right? So the, the bacteria that cause cavities digest sugars, carbohydrates, and they produce acids. But when they kind of like digest xylitol, they essentially starved themselves. Did that fit in and that reduces and less of those bacteria, which lowers your risk for tooth decay and cavities.
So that's like a really good intervention that we can recommend. But I think the other theme here. Again, like a lot of the products on the market, we've never really looked at them in the context of the effect on the oral microbiome. We've only looked at them in the context of, is this reducing the physical symptoms that we associate with conditions.
Right? So. Toothpastes or mouth washes that are targeted towards Gingervitis periodontal disease. It's always kind of a reduction in pocket that, which is the amount of space between your tooth and your gum line. But we're not, nobody's really looked at, is this reducing the bacteria that led to that condition in the first place?
Is it doing a better job of that than some other kind of intervention? And there's really no data on. The effects of certain dietary changes. You know, again like Listerine mouth washes on the abundances of these different bacteria in the oral microbiome. And it's really important because those bacteria are obviously directly related to your risk for oral health conditions.
But they're also related to a ton of systemic conditions as well. So the more spit you get in the mail, the closer you get to these answers. Yeah. That's cool. Send us your sped. And we can we back up a second and you mentioned Zola thought, can you, can you, and I hate to do this cause this is. Shooting myself in the foot, but can you talk about why sugar?
What happens when you eat too much sugar and why it leads to cavities? And why is that? It's almost like a sneaky solution there. Yeah. So sugar, I mean, The bacteria that cause cavities basically like ferment carbohydrates, right? And the by-product is different forms of acid that acid erodes the enamel and eventually institutes the, you go into the dentist and he is like, all right, you know, you did your x-ray, you've got a cavity come in for filling.
There are certain chemical differences between. Well, there's chemical differences between shutters in general, right. And xylitol has a certain chemical difference. I can't remember exactly what the difference is, but something about its structure means that the bacteria that normally consume sugars and fermented into acid byproducts, can't ferment.
Xylitol. So they don't produce the sugar, they just ingest it and they use the energy to go like, eat it, but they're not actually getting any nutrients. Isn't the right word. But for the sake of the conversation, they're not getting nutrients out of it. So they're not replenishing the energy they spent. And that essentially starts that.
It's a really effective diet drug for them. They're fast, effective.
Wait, did I read to you that there's fun guy like mushrooms in my mind. Like yeast. Okay, great. Yeah, we don't touch on the psychedelics industry yet. It's really bad. You can see little caps growing in. Okay. So like, sorry, go ahead. And max, and again, as, as much as I hate this argument and I hate this argument, is that why cave men had.
Okay. Teeth or you like, cause they're not eating as much processed sugar or whatever. Yeah. I mean, I think that that was part of it, right? Like there was, there's been a bunch of factors that have affected. I mean, I think like there's probably a lot of parallels between the factors that have affected our systemic health and our oral health.
So the switch to you know, like produced kind of unnatural sugars is probably one. I think there was a, a really interesting chart that I was looking at the other day. It was like the introduction of high-fructose corn syrup with obesity rates. In the United States probably see the same trend with a lot of oral diseases.
So I think that that's one piece of it. The other piece is a transition in the kinds of foods that we eat. So not necessarily the ingredients, but more so like the, the texture and structure for lack of a better term of foods. And there's a really interesting book called John. And I can't remember the author's name, but he's, he's a pretty well-known dentist out of Australia.
And it's all about the conversion from kind of like less processed foods that were, were harder to chew through, like really challenged your jaw to processed foods and the industrial revolution and how that completely changed the structure of the jaw. And humans because we're eating a lot softer foods, we're eating more sugars.
And basically that's led to like a pretty drastic restructuring of, of our oral cavity. And because the oral cavity has so many different environments and it it's basically created these opportunities for pathogenic bacteria to develop like new environments to grow and in our mouth. It talks about this in two James nester brings this up when he's talking about just breathing. Yeah. He says the same argument that, that our whole oral cavity and then including our nose, it's just sorta like sunken in and cause a bunch of problems, not just with our mouth, with our breathing. Have you found that like mouth breathers, people that snore a lot.
When they're sleeping, have more oral problems because of it. Totally. And I think that that, that kind of brings up a good part of the conversation where, you know, we've been talking about like sugars specifically as one factor contributing to the overgrowth of bacteria, but it's really a multifactorial because it is the environment that kind of allows these bacteria to thrive.
So when we go back to thinking about the bacteria related to tooth decay, they love. High acidity environments. Right? So they're producing acid because they liked that kind of environment in the oral cavity. They're a largely anaerobic species. So a lack of oxygen really does them well. They like, you know, so all of the factors that kind of create that environment in your mouth are going to contribute to your risk for oral disease and, and mouth breathing is one of those factors because you get a really drunk.
Kind of environment and your mouth and saliva is one of the primary mechanisms that your body uses to wash away a lot of the pathogenic bacteria. So a reduced salivary flow allows these bacteria to stick around in your mouth produce plaque, which is like basically, I mean, it's cement so that they.
Stick around even longer and better. And it also keeps them approximately close to your tooth, right? So they're not getting exposed to oxygen as much. And then when you introduce sugar to that environment, you're basically feeding them and you can imagine there's.
The more that I talk about that some more I'm like, man, I'm probably sounding like really gross and you guys are going to walk away from this like really concerned, but you can imagine there's like this layer of, well, there is a layer of biofilm on your teeth, but that biofilm is populated by all of these pathogenic bacteria.
So if you're eating sugar and you have this biofilm, they're going to be producing. And that acid is going to stick like right next year, too, because they're embedded in that biofilm. And that's just going to accelerate the rate of decay.
It's gross, but it's one of those gross ones where you're like, yeah, that's gross. Tell me more.
Yeah. I mean, also it's gross and moves me to act in a positive manner. I want to fix this. And I think that that's like, you know, the, I think the surprising thing for us was how many cases we have where it's not about. I think a lot of health companies right now are really in this optimization space.
Like how can we take people from five to 10 or eight to ring on your finger? I see, yeah, I'm probably zero to one on sleep. But
but you know, I think that there's this idea of like, what's. What's optimized. Somebody is exercise or let's optimize their diet. I think levels has done a fantastic job of conveying that message. And I think when we started the company, we thought that we would fall into that space as well. Like how can we help people optimize their oral health regimen?
But what we've actually found is like, it's really just getting people from zero to one because nobody. Nobody understands the impact that that simple hygiene practices have on their oral microbiome. And it's not because they haven't been told it's because we don't understand as an industry, we've just been telling people to do things without actually explaining why.
So, you know, one of the most compelling pieces of data that we have is we have four graphs and it shows the. The relative score for each of our kind of indication. So like tooth decay, gum inflammation, bad breath. And then the level of commensal bacteria and the bottom is flossing frequency. And when you go from like, I think it's times per week, so when you go from like zero to one to three, five to seven or seven or more going from zero to.
You know, like three to five times a week is a, I think on average it was a two and a half fold reduction for all pathogenic bacteria. And it was like four folder adduction for halitosis. Yeah. And it actually shows where I just read, I mean, watch to take talk that said flossing was a lie. Wow. So you have data that says we should be shoving doing okay.
I think that's kind of part of the, the that's one challenge that we're, we're tackling. Right? There's a lot of information out there. Yeah. I mean, I think that like, and I'm not going to sit here and say like, flossing is the cure all for oral care. Cause that's kind of part of the problem too. But like, you know, I think when, when you can show somebody.
Quantifiable data on how certain interventions affect their outcomes. It's, it's a, it's a really good tool to drive behavioral change and there's a lot less people, or there's a lot more people out there that floss a lot less than I would have thought. Before I started the company. I was in grade school when I saw a poster of Justin Timberlake on my dentist wall that said, That he flossed every day and I've flossed every day since I don't, if it was cause I was like, I want to make out with that guy.
That's why I need to floss. Or I want to be that guy. So I need to floss, but whatever it was, it was a great tool for behavioral change. So we should maybe do more of that. I think I want to get, I don't know. You guys remember? There's like some dumb cartoon when I was a kid, I students Danny Phantom and there was this guy like chip Skylar.
No, no,
but it was the same thing. I think he had a song, my shiny teeth and me. Oh, yes. Yeah. What's that? Yeah, it was fairly odd. Parents just don't like that. Yes. I know what you're talking about. It's catchy. It's a really well Gretchen song. I know.
Ah, okay. Well, interesting to know that, cause it was really recently and I was like, I've been flossing every day since grade school and I just learned that it was unnecessary. And now I just learned that I shouldn't get my facts from tic-tac good. Thank you. Yeah. Yeah. So, are there different types of diets that you suggest?
Is there one out there that's best? Should we all be keto for our mouths? You know, I think I think that's the exciting thing about the oral health space. We have. We don't know the full effects of diet yet. Like we don't know if a ketogenic diet is going to be better for somebody than paleo. We do know that avoiding sugar.
It's generally a good idea, but it's nothing new, obviously. We're starting to find some trends between certain foods, so we know. A nitrate rich diet contributes to better, you know, more abundance of the beneficial bacteria. There's a really interesting correlation that we're investigating between certain species of bacteria in your mouth that reduce nitrate into nitric oxide and blood pressure levels.
So I think so a good amount of nitrate reduction happens via the bacteria in your mouth. Nitric oxide is reduced to lower levels and blood pressure. And we've been investigating kind of the correlation between people that have high levels of those bacteria versus low levels. And it seems to line up really well with blood pressure status.
So the idea is. You know, if you're, if you're somebody who's battling high blood pressure and you're taking a lot of nitrate supplements, but you don't have those bacteria in your mouth, like you may be getting kind of diminishing returns on that intervention. So if we can increase the abundance of those bacteria may be more effective in, I mean, not only helping your oral health, which is great, but also lowering your blood pressure.
Yeah. Interesting. Are there other things like that as it going to be to the point where you're taking my spit and then you can, you know what my weight is and if I'm vegan and my religion and how attractive I am, if you saw it, you send a picture. But no, I mean, we yeah. There's a lot of information and in your spirit. And I think we're really just scratching the surface. So another thing that we're investigating as a company is there in the dental industry, like there have been clinical associations. I call them like clinical anecdotes, where if you talk to a hundred dentists, 99 of them will tell you like, All of my diabetic patients.
No, that's nine out of 10 or all of them will say like my diabetic patients have way higher prevalence of gum disease. Right. And they'll swear by the association. There's been a ton of studies looking at it just from the characterization level, but there's been very little research, actually establishing a mechanistic relationship between oral.
And metabolic health, I guess, to use like a more general term. And we know that oral health is rooted in the oral microbiome. So there's, there's probably an interplay of the bacteria that are in our mouth and our metabolic health. And we'll be able to kind of get some insights. I don't, I don't know if we'll be able to tell you exactly like what your What your A1C levels are, but we'll at least get some kind of directionality around, you know, maybe you're pre-diabetic or you're at risk for becoming pre-diabetic or something like that.
And we're seeing similar associations across a pretty wide range of conditions. So neurodegenerative diseases, there's been a lot of investigation between ki Jinja VALIS, which is like one of the most prevalent bacteria associated with gum disease. And Alison. And there's been a really kind of well-established relationship between those two.
And then we've also found some associations between the oral microbiome and gut microbiome dysbiosis. Oh, wow. Interesting. So yeah, I mean, it's all connected and why am I surprised? Oh, that maybe there is kind of like a, at some point, maybe we can tell. If somebody is on a kosher diet and I could, yeah. And you could tell,
is there a lot of crossover with the microbiome, meaning your mouth versus your stomach versus we have one on our skin too, right? Yeah. I think the mouth is, is really unique. You know, we, we talk about the mouth internally as the gateway to the body and the mirror of our health. So there's, like I said, there's been a lot of relationships established between systemic health conditions and oral health.
Gum disease may be a co-morbidity or really like in some cases, a symptom of an underlying issue going on somewhere else in the body. And it works in the opposite direction as well, where the pathogenic bacteria in our mouth is can migrate to other parts of our bodies and cause issues there. And it's not just a pathogenic bacteria in our mouth, sometimes beneficial bacteria in our mouth become pathogenic and other parts of our body.
And we've, we've started to see a lot of cases of that. So you know, I think certain bacteria in the oral microbiome has been implicated in colorectal cancer. F nuclear atom is I think the specific species and most of the research I've seen. Like I said, there's been associations with peach and Dallas where that bacteria can kind of make its way to a CSF and then cross the blood-brain barrier.
And then it produces something in our brains that kind of leads to a cascade effect of the biomarkers that are associated with the progression of Alzheimer's disease. Well, I need to brush my teeth. Okay.
So yeah, we talk about how diet and lifestyle can affect and maybe even like how you're sleeping, but what about like DNA? Is there something that like, I was just born with that my mouth is going to be a certain way. Are you looking into that kind of thing? Yeah, there's, there's a couple of factors in there.
So, like I said, the. You know, there's differences in the structure of one mouth compared to another, some people have dApps and their teeth, the word misalignment or whatever. And each of those changes introduces like a, a very distinct environment and the oral cavity. So. You know, if you have a gap in your teeth, maybe you're more prone to bacteria that can grow in that area that are pathogenic and lead to a higher rate of gum disease.
We've been looking at the effect of orthodontic appliances, so like braces versus clear aligners. So the interventions that are associated with those With the rates of, of the growth of those bacteria. And I mean, ultimately like the structure of your mouth is rooted in your genetics. So that's, that's been a really big part of it is kind of understanding, are you predisposed to having this alignment in your oral cavity or are you predisposed to maybe having like weaker enamel compared to somebody else?
Because that's another really big factor where if you have. I'm using very like broad terms, but if you have strong enamel, you might be able to withstand a higher abundance of those cavities causing bacteria than somebody with really weak enamel. And that shows that physiologically and whether or not you get those symptoms.
Yeah. That is the teeth. Have you seen any teeth structure? Yeah. Yeah. So we've been, we've been looking at people that have been. Like, like pre clear aligner treatment and post clear aligner treatment. And there's definitely a difference in the makeup of the bacteria that are present in the oral cavity.
I don't know if it's enough to say. We haven't been able to quantify the difference in like risk for disease for those people. But it obviously introduces different kind of niche habitats that pathogenic bacteria can grow in. So we're starting to see and understand patterns of like species that might grow between different people.
Another factor to consider is like when you have those intervention, a good example is like a night guard. So. You're you're wearing this thing, like in your mouth for a bunch of hours every night, kind of take it out and you just leave it there. No, no, no swish swish it. So we're starting to, you know, we're, we're still looking at this, but we're starting to see.
Bacteria that really shouldn't be in your oral microbiome at all that are there. So it kind of these like non-canonical oral bacteria that are good and new good one. Yeah. That I'm introducing by.
It wasn't clear by my expression. I wear a night guard every night, actually. Yeah. I want to ask a self self-serving question. Is there a connection to your microbiome and gum recession? Because I have this problem and it's, I have supposedly because I'm clenching and that's why I wear the night guard, but maybe there are more factors.
Yeah. I don't, I need to look into the clenching and gum recession piece, but I mean, Gum recession, like in and of itself is really tied to the bacteria that cause gum inflammation. So gum recession is the result of these bacteria causing like an immune response by your body. It leads to the inflammation and then eventually your body starts kind of like.
Eating away at your bone and tissue structure. And that is kind of what spurs gum recession, as far as I know. So reducing the bacteria is kind of like the ultimate goal. I think, you know, maybe the, maybe the idea behind it was, we do see a lot of Parallels between clenching your teeth and like an increase in the amount of pathogenic bacteria.
I'm still trying to understand exactly like why there's a correlation. I don't think it would be as distinct as something like mouth breathing. Cause it's not fundamentally like changing the environment, but has been something that we've seen. So that would be the introduction of the night guard, but it would be worth figuring out if you're introducing anything else.
What the hell? It sounds like I had this problem. And then they gave me something to make the problem worse. You know what it is? My stress dreams are feeding bacteria. They're just eating my uni, but I think that's, that's another important point is like in the dental industry, you know, you're only as good as like the tools and the data that you have available.
And I think that that's been a really big gap in the standard of care and it's not necessarily. We're not pointing fingers at anybody, but there is this amazingly advanced technology called sequencing that's existed and has been like brought into the realm of healthcare for the last 10 years. But in largely in dental care, like we're still relying on x-rays and observational screenings and questionnaires that really are just getting at the latest stages of diseases.
And they're not really. They're not getting to the root cause of what's actually driving your condition. Right? If you have a cavity, like that's just saying that you have bad enough to CAE that like, you know, one or more of your teeth has a hole in it. With gum disease, we're only looking at the resulting kind of effects of these pathogenic bacteria.
And we're using that to characterize and make decisions around the interventions that we introduced. By using the oral microbiome, we can get early detection. We can really understand the specific species that are driving those conditions and we can monitor like exactly what those levels are as you introduce new interventions.
So the whole point is kind of pre visible symptoms, pre anything going wrong. Can we just get you back to baseline and keep you there? Yeah. So it sounds like you're also retesting after the interventions. Is that a part of this. Yeah, we highly, highly recommend it. Some people are just like, I haven't seen a dentist in 10 years.
Like I just want to know that everything's okay. And, but I would say for people that are actively trying to improve the best way to understand, like how different things are contributing is. Yeah. Well, and how, how much does your mouth evolve over time? Like, is it different if I send you my spit next week, will it be different than this week or like three months from now?
Or even like morning to night? How it'll show. Yeah, so we we've done a couple internal studies, like rapidly doing testing. So we'll do like three samples a day or something. Over the course of the couple of weeks and the oral microbiome shifts. I think that there's a difference between like the noise of shifts day-to-day and what actual signal evolves into in terms of, you know, are you week over week or month over month.
On a trajectory towards some kind of negative health outcome. And, and we're starting there. There are definitely going to be differences in your oral microbiome day to day, but we can generally we can get like the root signal from any kind of time point. There's not going to be so much of a difference taking your sample today versus next week that it throws off like your core results.
Okay. And unless you started using mouthwash, there's no one at Brasil used mouthwash. I don't think so. I would be surprised because we had a fatal.
I have once a day. Right? Or is it now? I got to do in the morning too. I do. I do once a day. I got to go make a tick talk. Yeah. And the word out there.
What's the future for Bristle? Where, where are you headed with all of this? Yeah, I mean, I think You know, the future for Bristle, the statistic that always comes back to me and almost every conversation I have is like cavities and gum disease have been the most prevalent conditions on the planet since 1990, I think.
And they're preventable. Like we're not talking about some mysterious set of diseases or yeah. Some kind of code we have to unravel like, like cancer, like these. We understand the root cause of these conditions like we have and can develop a lot of the tools to tackle them. And then we know that there's associations between those conditions and systemic conditions.
So for Bristle it's, you know, can we kind of like reinvent the way that we approach our oral health? Can we. In a more precise and personalized and preventive manner. And, and our big bet is that if we can get everybody from like zero to one on their oral health and make a really big impact there, we're going to see meaningfully improved overall health conditions coming out the other end.
So for us, it's, you know, let's build up the database. Let's really understand what drives these conditions and how we can solve for oral health conditions. Now, get that out there to everybody we possibly can. Start investigating some of the more mysterious connections between our oral and overall health.
And, and eventually, you know, we really want to migrate to this 360 degree view of what's going on in your body, all from a saliva sample, which sounds very fair and OSI when I say that out loud, but it is kind of what we're working towards as a company. Solid. Yeah. I mean, the reason Theranos took off is because we all wanted it.
So don't feel bad about saying you're doing it.
And I imagine the goal too, would be, yeah, like you're saying ubiquitous use of this. So hopefully insurance will be covering this P this preventative kind of thing. Yeah. I don't know how much you've dealt with dental insurance. It's a it's identity. It's actually my godfather. I see him all the time.
Yeah. I mean, I think that that's, you know, the same gap that exists between the technologies that are available in what's being implemented in dental care. I think.
Disparity, I guess is maybe a better word exists between like our healthcare model and the incentives that we use for medical healthcare and our dental care model and the incentives around that. So medical healthcare. You know, you have your deductible and everything after that insurance covers, it's the inverse for dental insurance.
You, you kind of have a maximum, it's usually like 1500 or 2000 bucks a year. There's a couple like services included. And then anything past that you're paying out of pocket. And. Like one procedure generally gets you above whatever that maximum is. We we've heard stories from our users about, you know, I could only do one, the two procedures that I needed this year and I to wait a year for my dental insurance to like renew because they couldn't afford it.
So another. You know, another statistic that I love to throw out is we spend, I think it's like $150 billion a year on dental care as a country, which is like a tiny proportion of the $3 trillion of total healthcare. But we, 40% of that is actually an out of pocket expenses. It's like 10 times higher than any other area of healthcare.
So. On paper, like it looks like we're spending the least, but as patients where we're actually spending the most on, on our dental care. And again, this is like for preventable conditions. So our, our goal as a company is like, I think that there is, I think oral health is probably the lowest hanging fruit in terms of like how we can really impact people's health and the healthcare system.
And we have this opportunity to rebuild it in a way that I think makes sense for people. So that's, that's our goal as a company is like, this is a solvable problem. We have the technology exists. There's not some like crazy space X type, you know, development that we have to do. So like, let's go, let's go do this the way that it should be done.
Thanks. Appreciate you doing that.
Well, sweet. And where can the fit heads go? Find more about Bristle. Yeah, you can check us out at bristlehealth.com. We've got a bunch of. Potentially, I guess, scary blogs from some, some good news to you. Yeah. So go check us out. Personal health.com and it's personal health for all of the typical social media channels.
We're just building out our tech talk so you can go there for sure.
Awesome. Thank you so much. It was great. Yeah. Thanks for having. And thank you to the fit heads. If you can rate and review on apple, that helps us out a whole lot. And we'll see you next week.