How Our Oral Microbiome Informs Our Brain And Heart Health Status, And Risk For Disease, with Danny Grannick
BrainFirst Radio
60 Minutes
Episode Transcript
Ramon David (00:00:10):
All right, hey it's Ramon, and Welcome to BrainFirst Radio,science-backed strategies, insights and tools you can use to upgrade your brainand life. Now, let's get into the episode. No interruptions, enjoy my friends.Welcome to the show. It's great to have you here.
Danny Grannick (00:00:27):
Thanks, it's great to be here.
Ramon David (00:00:30):
So, you are the co-founder of Bristle Health, right?
Danny Grannick (00:00:36):
Correct. Yeah, co-founder and CEO.
Ramon David (00:00:40):
CEO. So just explain for our listeners, first of all, whatdoes Bristle Health do?
Danny Grannick (00:00:46):
Yeah, so I think to put it very concisely, we really helppeople measure, understand and improve their oral health. And we do thatleveraging the oral microbiome. So the makeup of bacteria, fungi, and virusesthat reside in your oral cavity. We analyze saliva, understand what kind of microbesare in your oral microbiome and that directly informs us as to what your oralhealth status is and risk for disease.
Ramon David (00:01:16):
Right, so gut microbiome, hot topic at the moment, we'vehad, I mean, a bunch of guests on, from Emeran Mayer to Christine Béchar,talking about the gut microbiome, but oral microbiome, not something that a lotof people are talking about. Unless you're kind of in the biohacking field.
Danny Grannick (00:01:38):
Yeah, I was, I think we've always been kind of surprisedthat the oral microbiome has been, I wouldn't even say secondary, like reallyit's far down the list, right? Gut microbiome, skin microbiome, vaginalmicrobiome, which was surprising to me because I've done gut microbiome tests.And in terms of sample collection, the oral microbiome is definitely myfavorite so far.
Ramon David (00:02:09):
So, how did you get into this yourself? What's thebackstory here?
Danny Grannick (00:02:17):
So, our founding team, we all come from different areas,but the common piece is we all have a background in genomics and sequencing, soin one way or another. I come from the commercial side of genomics. Our CSOcomes from the research side, and I think it was really a case of being theright place at the right time. Genomics has obviously been gaining inpopularity. Companies like 23andMe and Ancestry have gotten it more into theconsumer side. And then we've seen an explosion in using genomics clinically.So we're starting to use genomics for early detection of cancer. We're doing itfor predisposition for other systemic diseases. And I think in the same veinwe've seen a really big shift to using other kinds of technologies, so likewearables to start to quantify other aspects of our health and use that to informpreventive strategies and behavioral changes that we can make to mitigatefuture risk.
Danny Grannick (00:03:19):
So, we'd seen kind of this explosion in all of thesedifferent applications and ways that we could improve health. And I think itwas just a conversation that I was having with my co-founder, well, my nowco-founder, then friend, and he is, I think this cliche case of being religiousabout oral hygiene and inevitably having cavities every time he would go to thedentist. And he had a dental appointment the next day, he was complaining andkind of venting to me about it. And I was sitting there on my high horsebecause I wasn't the best about oral hygiene, but for whatever reason, I neverhad issues going to the dentist and really had very few cavities for my entirelife. And having worked with gut microbiome companies and having seen whatgenomics could do it, it kind of hit us in the face. And we started lookinginto the existing research around the oral microbiome and basically uncoveredthat we've known for decades that cavities and gum disease, the two mostprevalent diseases on the planet since 1990 are rooted in the oral microbiome.
Danny Grannick (00:04:38):
There's a subset of 12 or 13 pathogenic bacteria thatdirectly cause these diseases. And naturally we started trying to see what wason the market around it and really found nothing. The oral care and dentalindustry has I think been relatively stagnant. When you think about your visitto the dentist, you go in, they do an observational screening, they'll do anx-ray, we're looking for the presence and severity of physical symptoms relatedto existing disease. And we knew that sequencing could detect these microbesmuch earlier. We'd seen it done with the gut microbiome. And that was reallythe starting point for the company was, can we shift the standard of dentalcare from this very kind of reactive procedure first, model of care intosomething that was preventive?
Ramon David (00:05:35):
On the genomic side, is this something that you've alwayshad an interest in? What was your entry into this space?
Danny Grannick (00:05:43):
Yeah, my background's in biochemistry. I grew up in SanDiego, so Illumina, which is kind of the giant in genomics was in my backyard.So I was exposed to it pretty early and I had started my career there. I thinkpersonally I've always been kind of an inch deep mile wide scientist, whichisn't great if you are planning to go get your PhD. So I jumped on thecommercial side and started working just kind of across the industry. And itwas that exposure I think that really led to kind of stumbling onto this ideafor Bristle.
Ramon David (00:06:21):
So, oral microbiome and oral health, what do we need toknow? Because I think again, for a lot of our listeners and maybe some of themare a little bit more familiar with this, but I'm going to take a guess and saythe majority of us, not so much, and oral microbiome, oral health, my firstthoughts that come to mind are, okay, occasional trips to the dentist forcheckups. I do a few basic things like oil pulling and those sorts of things,but what do we need to know? Where's a good place to start here?
Danny Grannick (00:06:59):
Yeah, there's so many places. I guess we can start withthe history, I think the history of the oral microbiome is really interesting,ignoring kind of the oral health piece for now. I can't remember exactly who itwas, but some of the first bacteria that were ever observed actually came fromthe oral cavity hundreds of years ago. So in a lot of ways the oral microbiomewas actually one of the starting points for microbiology as a practice. Andover the decades there was more and more research looking at the role of thesespecific pathogenic microbes as they related to oral disease. You can imagine hundredsof years ago oral health wasn't great. People were losing their teeth all thetime. And the mouth is this just exposed component of our bodies. It getsexposed to pathogenic bacteria, gets exposed to your beneficial ones. So itreally is kind of a breeding ground.
Danny Grannick (00:08:03):
If you're interested in microbiology and all of a suddenit becomes this relevant, scientific topic. So the amount of kind of basicresearch, I think wasn't necessarily looking at the connection between the oralmicrobiome and the oral health. It was actually just using the mouth as areally easy entry point to start building the foundation of microbiology as apractice. Fast forward a couple 100 years, and people are starting to realizeand identify specific bacteria that are related to oral disease. And if we lookat kind of the big two, cavities and gum disease, there's a subset of, let'scall it 20 bacteria. And just for easy math, 10 might be related to periodontaldisease or gum disease, and 10 might be acetogenic. So they produce acid andthat acid decays your teeth and eventually leads to a cavity.
Danny Grannick (00:09:01):
And that was kind of where the science stopped I think fora really long time. Like we were aware of these bacteria, they're commonlyknown as [inaudible 00:09:10] orange complex, and dental school students aretaught about this when they're getting their degrees. You can find a bunch ofresearch online about this subset of bacteria, but for whatever reason, thoselearnings weren't really translated into clinical care. And I think that theremay be some interesting underpinnings with the origin of dentistry as apractice. We know that it started in barber shops, it's kind of this verysurgical, almost engineering focus practice, but for one reason or anothermicrobiology and really kind of that start never made its way into the way thatwe assess oral health.
Danny Grannick (00:09:53):
So, fast forward another couple of decades to today, andwe have this amazing technology, genetic sequencing, next generation sequencingthat allows us to expand our scope and detect all of these bacteria. And we'refinding that surprise, biology is a lot more complex than we ever thought itwas. And going back to the oral cavity, we have been able to uncover that themakeup of microbes in our mouths are way more diverse than we ever imagined. Soit's not just those 10, 12 or 20 bacteria related to disease, there's actually700 plus bacteria that had been associated with the oral microbiome. And onaverage, each of us has anywhere from a 100 to 250. And I think each of thosebacteria has a role to play. We kind of had the same assumption with RNA for awhile, kind of, or sorry, non-coding DNA, like junk DNA. We didn't think thatit did anything for years, and now we're starting to see that it plays a reallyimportant role.
Danny Grannick (00:11:06):
And I think we're starting to see the same thing with theoral microbiome. So we've gone from kind of this idea of 20 bacteria that wererelated to disease to 700 bacteria, but we don't know what they do. And a lotof the research in the last couple of years has uncovered the role of thesebacteria in not only our oral health, but our overall health. And I think areally apt description that I've heard is, on the one hand our mouths are kindof like a gateway to the body, so they can let pathogenic bacteria pass throughinto our body and that can increase our risk for systemic disease. But at thesame time, our mouths can also be more like a mirror and reflect changes thatare going on in other parts of our body. And we've seen that quantitatively andqualitatively in the microbiome.
Ramon David (00:11:59):
Hmm. So what sort of impact does this have, what sort ofimpact does the oral microbiome and the bacteria have on things like youmentioned systemic disease, perhaps if things like brain health, cognition,these sorts of things, what do we know so far?
Danny Grannick (00:12:18):
Yeah, so again, for the past couple of decades we missedthe bridge between the discoveries of the oral microbiome and putting it intoclinical practice. So when you go through the literature, there's a lot ofassociations between poor oral health and systemic disease. Poor oral healthkind of being that surface level understanding, right? So we know that aspeople age, their oral health declines and cognitive decline also happens atthe same time. And there's a correlation between populations. But again, therewas never kind of a deeper understanding of why, or if those two are connected.We see the same thing with declining oral health or the prevalence of gumdisease and hypertension and cardiovascular disease. Again, clinicalcorrelations, I call them clinical anecdotes. If you talk to a 100 dentists, 99of them will tell you, "Of course, my patients with heart disease have wayhigher prevalence of gum disease."
Danny Grannick (00:13:25):
But it was still something that nobody ever really kind oflooked into. And we see the same thing with most chronic conditions. Diabetesis also in there. And the oral microbiome is that bridge between the two. So wehave found that specific bacteria in the oral microbiome that are connected tooral disease, I think one of the most notorious is P. Gingivalis, has also beenimplicated in cardiovascular disease, so specifically Infective endocarditis.And it's also been implicated in Alzheimer's, so cognitive decline. And that'sone example of 150 bacteria that are residing in our mouths that are tied toconditions that are outside of the oral cavity.
Ramon David (00:14:15):
What, just talking about the literature for a moment, arethere many intervention studies out there demonstrating certain effects? What'sthe state of the literature?
Danny Grannick (00:14:26):
Yeah. So that's been another kind of interesting piece.There have been numerous studies looking at the impact of preventive dentalcare and improving again, kind of top level idea of oral health with reducedoverall healthcare expenditures. There was, let's see, Kaiser in the PacificNorthwest, as well as Cigna had both performed clinical studies. Looking atpatient populations, I think both of the patient populations were diabetic. Andthey looked at people diagnosed with diabetes that also had periodontaldisease, and the impact that more consistent dental care and the reduction ofthe severity of periodontal disease had on their overall healthcare costs. Can'tremember the exact numbers. But I think the average between the two wassomething like a $1,500 per year reduction in overall healthcare expenditures,ignoring the dental piece, just getting people that preventive dental care andimproving their oral health.
Ramon David (00:15:28):
Yeah. Yeah. What sort of preventive dental care are wetalking about? To what extent are they taking this in the research?
Danny Grannick (00:15:38):
It's pretty shallow. It's really just getting people intothe dentist twice a year and making sure that they get cleanings. And I thinkthat it touches on one of the most pervasive problems with oral health, whichis, nobody really thinks it's important that they [crosstalk 00:15:55].Exactly, I mean, if I was sitting here talking to you and all of a sudden myhands started bleeding, that would be an emergency to me. Like that's a signthat something's wrong, but when we brush our teeth and there's blood in thesink, you kind of just ignore it. And I think that a big part of that is ... Ineed a toe line here, but the dental care experience isn't comfortable and it'snot enjoyable and it's something that people try to avoid. And I think thatinstead of using dental care as a barrier to improving your oral health, whichis what's currently going on, like let's eliminate the barrier and focus onjust making it really easy to improve your oral health at home. And we'll seeall of these improved outcomes on the other side.
Ramon David (00:16:50):
Hmm. What are some of the studies that you would like tosee being conducted in this space?
Danny Grannick (00:16:59):
So, the easy ones. I mean, I haven't seen a study outsideof the research that we are doing that has quantitatively shown the impact ofbrushing and flossing on pathogenic bacterial load in the oral cavity, whichyou would think is pretty important and something that you would want to showif you're a company selling those products. So, at kind of the highest level, Iwould love to see more research around the impact that zero to one behavioralchanges in oral health can have on oral health outcomes. As a company we'recontinuing to build our database, and I think that there are some reallyinteresting questions to ask. There was a study done, let's see, in 2018 Ithink, and I'll send you the paper, but they uncovered, it was kind of thefoundational study that uncovered P. gingivalis in the brains of Alzheimer'spatients. And the ideas that P. gingivalis produces a toxin called gingipains,and gingipains are going to influence the creation of [inaudible 00:18:11]beta-amyloid proteins, and that's related to the onset of Alzheimer's.
Danny Grannick (00:18:18):
But I think that that theory and that hypothesis isrelevant across all of these different indications. And all of the research todate has been in really small patient populations. It's more of a proof ofconcept, but I would love to see again more quantitative research identifyingthe role of bacteria in the oral microbiome as they relate to heart disease andAlzheimer's and diabetes. Because the more research that we can do, the morelikely we are to uncover the mechanism of action, and we can create theinterventions that we need to potentially make a huge dent in some of the mostcommon chronic conditions on the planet. We've seen two companies that I knowof, two therapeutics companies spring up in light of that original researcharound Alzheimer's. Protexin and Keystone Bio are both developing therapeuticcandidates that are targeting P. gingivalis or gingipains. And it's not to cureperiodontal disease, it is to slow the progression or stop Alzheimer's.
Ramon David (00:19:23):
Yeah, super fascinating. Talk to us about some of these... I want to find out more about the company and the tests that you're runningand what you're doing there, but first of all, I think it's important to goover some of the practices that we currently have. I'd love to hear yourthoughts on everything from ... Why don't we start with what's a common one,fluoride, right? No neurotoxin, but also we know the dose makes the poison. Somany people are anti-fluoride. So many people are pro-fluoride. What are yourthoughts? What does the literature say? Where are we at on the fluoride debate?
Danny Grannick (00:20:07):
Yeah, that's a really good question. I mean, it'ssomething that comes up with, it is a hot topic. And my easy escape answer is,I don't know what the long-term effects of fluoride exposure are, becauseagain, I don't think that there's been enough research quantitatively showingwhat those effects become. I think if we're just focusing on the oral cavity,fluoride's been shown to strengthen enamel and reduce the rate of cavities. So,if you are just a mouth, it sounds great. I think that just like other areas ofbiology there are downstream effects. And until we really measure what thosedownstream effects are and we understand what the implications of usingsomething like fluoride and having that consistent exposure through our waterand through our toothpaste and its relation to concentration, I think that wehave to be aware of the potential negative side effects.
Danny Grannick (00:21:13):
It's tough because a lot of the existing research, thereis a clear advantage to using fluoride when it comes to protecting your teeth.And I'm comfortable saying that I think the neurotoxicity I need to look intomore. And I think maybe the most exciting part is that a lot of oral carecompanies are investing into materials outside of fluoride that are just aseffective. And my short answer is, if you're not comfortable using fluoride,there are alternatives that have been shown to work as well or better thanfluoride. I think the CDC is coming out with something pretty soon though.
Ramon David (00:21:55):
Okay. Yeah, I was going to ask, what are the alternativesto fluoride and are they as good? And can they be localized to having an effectjust on the teeth without having effects on the rest of the potentially nervoussystem and the rest of the body?
Danny Grannick (00:22:13):
I think so. Nano hydroxy appetite has been one of the kindof touted ingredients as an alternative to fluoride. And I think it mimics andit spurs enamel production in a lot of ways better than fluoride does. I thinkfluoride is more of kind of like a protective material where this is morefocused on regeneration. And it's not in our drinking water.
Ramon David (00:22:44):
Yeah, right. What about oil pulling?
Danny Grannick (00:22:50):
We're doing a lot of the research around that as well. Ithink with a lot of the things that are coming out, and we might as well throwactivated charcoal toothpaste in there as well. There are a lot of things onthe market that are making some pretty significant claims as to what they cando with regards to your health or your oral health. And I haven't seen the hardscience backing up those claims, in the way that I think I would want to see.And that's one of the goals of Bristle is, with every test that we do weessentially create a new data set or at least a new data point. And we thinkthat we'll be able to start publishing a lot of objective results around theefficacy of some of these practices.
Danny Grannick (00:23:40):
Oil pulling, I don't think it's bad. I don't know if it'sthe one thing that everybody should be doing to improve their oral healtheither. Charcoal toothpaste. I don't know if it's bad. I do know that it is apretty harsh material to be using on your teeth and it can increase your riskfor cavities. But there just hasn't been ... I don't think that there's been acheckpoint created or some kind of universal standard for determining howeffective a lot of these oral health products and recommendations are, andthat's kind of where we want to be.
Ramon David (00:24:17):
Yeah. And I'm not sure whether they ... I would imaginethere are big differences in the different types of activated charcoal, but I'mimagining that some could be a lot more abrasive than others. And is there arating scale for that like there is with toothpaste? It's quite an unregulated,I suppose it falls into the sort of supplement category I would imagine, theseactivated charcoal products.
Danny Grannick (00:24:42):
Somewhere, it's somewhere in there. I mean, yeah it's, andI think the other question too is, there is an abrasion rating for toothpaste.I had never thought about how abrasive the toothpaste I was using before Istarted Bristle. So I think the other big kind of challenge is, if we do comeup with some kind of rating system and we do have this objective information,how do we make sure that people are aware of it and they're using that to informtheir choices when they go looking for a solution?
Ramon David (00:25:15):
Yeah, yeah. I remember looking for the abrasion rating forthe different toothpaste that I was looking at using, this was many years ago.And it was very difficult to find. There was only a few of the top kind ofbrands that you could get hold of that information at the time. I don't know ifthat's changed now, but it's not like you pick up a toothpaste box, at leasthere in Australia, and you see the rating on the box or anything.
Danny Grannick (00:25:41):
I think that's, it's a theme, I think throughout oral careproducts, where there's not a lot of information beyond a few words on the boxthat really inform you as to what the best product is for you or whatever yourcondition is. There's people will put teeth whitening toothpaste. What doesthat mean? What is in there that's making it better, a higher abrasion. Maybethat's just scraping more stuff off of the surface of your tooth. There's guminflammation reducing toothpaste. But it has the same ingredients as the toothpain reducing toothpaste right next to it. So I think there's a big misunderstandingin what the difference is between oral care products. And there's not a lot ofguidance when you go to a store and you're looking at a wall of like 300 tubesof toothpaste to tell you, "Which one is actually going to address what Ineed?"
Ramon David (00:26:50):
What about flossing? That should be part of regularpractice every day, twice a day.
Danny Grannick (00:27:00):
Yeah. The data that we've seen suggests that flossing is agood oral health practice. I think just like everything else, flossing thecorrect way is as important as doing the practice itself. A lot of people dothe towel kind of, let's really get in there and clear out everything we can.And that's actually not, I think procedurally the right way to floss yourteeth. It's not supposed to be this, I'm trying to think of the word, but I'msure anybody listening can imagine what I'm talking about. It is supposed to bea really gentle procedure. The idea is not to try to squeegee the hell out ofwhatever's between your teeth. The idea is to expose these anaerobic pathogenicbacteria to oxygen, which kills them. And you don't need to go up into your gumline, bordering on a self-lobotomy to do that.
Ramon David (00:28:04):
I'm imagining when you're doing this action and for peoplewill be watching parts of this video if we clip this and end up putting thisclip on social media of this segment just here, you'll see the action. I'mreminded of the old school guys would have cut into trees, and they've got oneguy standing on one side of the saw and one guy standing on the other side ofthe saw, and they're hacking back and forth into-
Danny Grannick (00:28:29):
Yeah, I need to, I'm going to use that. Yeah, that's a waybetter description. Post that one, not mine.
Ramon David (00:28:39):
All right. So flossing, be gentle, obviously brush teeth,fluoride. We have some alternatives, oil pulling. Maybe, maybe not. Any otherpractices that we need to be incorporating on the mouth side before we get tothe diet and lifestyle side of things?
Danny Grannick (00:28:58):
Yeah, I mean, I think it's worth calling out mouthwashwhile we're kind of on this topic. Mouthwash, and it's interesting, I mean,I've spoken with people that are religious about their gut health, will nevertake antibiotics and use mouthwash every day.
Ramon David (00:29:22):
Yeah.
Danny Grannick (00:29:23):
And they don't realize that two liter bottle of mouthwashthat says kills 99.9% of bacteria related to gingivitis, that's wiping out youroral microbiome completely. And it opens up the gates for a lot of thesepathogenic microbes to then move in. It's the same stance as antibiotics. Thereare some better mouth washes out there that don't wipe out the oral microbiome.But I mean, I think again, kind of in the same trend, one of the big problemswith oral care products right now is they're broad spectrum and relativelyineffective. They kind of work for everybody, but they don't really work foranyone.
Ramon David (00:30:13):
So let's talk about some of the things that I know manypeople wouldn't consider in the same sort of sentence or in the same realm asoral health. So most people will be thinking, "Yeah, I brush my teeth. Ifloss my teeth. I go to the dentist a few times a year." What about theimpact of diet and lifestyle?
Danny Grannick (00:30:37):
Yeah, I mean, that's another kind of surprising piece tome where we can focus on diet first and then move on to lifestyle. But it's asurprising thing. For some reason the mouth just seems to get left out of theequation, for any decision that anybody makes. And with diet, I think part ofit is just, again, first of all a lack of research, really connecting certaindietary changes to your oral health outcomes. Everybody knows that sugar leadsto cavities, but there are a lot of other insights related to your oralmicrobiome that can impact your oral health and your overall health as well. Soa really good example, there are a subset of bacteria in the oral microbiomethat are nitrate reducing bacteria. And the more nitrate reduction you can do,I guess nitrate reduction is tied to a lower risk for heart disease and lowerblood pressure.
Danny Grannick (00:31:48):
The bacteria in your oral microbiome have an enzyme thatperforms that action. That enzyme is not natural to the human body. So if youdon't have those microbes that can perform that function, you can't reduce thenitrates in the foods that you're consuming. And the lack of those bacteria'stied to higher blood pressure. So understanding what's in your oral microbiomeand what's not in your oral microbiome may lead you to change your diet and notonly improve your oral health, but also reduce your risk for heart disease inthe future. There's a lot of other examples, the kinds of foods we eat. Therewas a really good, I think he's based out of Australia. There's a really goodbook called, Jaws and the author, I'll need to look it up. The authordescribes, of course I type in Jaws and the movie comes up. I should havethought that one through. Let's see.
Danny Grannick (00:33:00):
So, the author talks about the Industrial Revolution andits impact on oral health. So the idea is, before the Industrial Revolution wewere eating a lot of chewier foods. We were using our jaws more to kind of eat.And post Industrial Revolution when we were able to start processing foods,everything got a lot softer and switching the texture of our diet actually hasimpacted the way that our jaws grow over time and it shifted our teeth. And oneof the other really interesting things about our mouths is, it is unlike thegut I think it's not just one environment. There are a ton of differentsub-environments within the mouth that each harbor different kinds of bacteria.So the change to our jaw structure introduces new environments that may favorpathogenic bacteria to grow in. And a lot of that has to do with thishistorical shift in the way that we've processed and consumed food.
Ramon David (00:34:26):
So, sugar, bad. I mean, let's be honest. We all know that.What about some things that we may not have thought about, like refined carbohydrates,breads, cereals, these sorts of things? Do we know, is there any impact therefor over consuming a lot of these types of refined products?
Danny Grannick (00:34:52):
And I'll say that with the caveat, it really depends onthe individual's microbiome. So specific bacteria can metabolize certaincarbohydrates and not others, right? So for some people eating certain kinds ofcarbohydrates may not be a big deal. There may not be the production of acid inyour mouth that leads to cavities, whereas for somebody else, it might. But Ithink, the first step is understanding what those bacteria are, because we cancharacterize exactly what those bacteria metabolize and that can help informdietary choices going forward. I think the really exciting thing is if we canshift that community, whether it's through prebiotics, probiotics, phagetherapies, we can open up new dietary options for people or get them thenutrients that they may not have access to right now.
Ramon David (00:35:45):
Yeah, yeah. I think that's one of the things with thebehavior change and the discussion that I often have with friends and familymembers around even things like electric cars. It's like there's, most people,if presented with an alternative to some gas guzzling environmental disaster ofa motor vehicle, they would choose the better option, right? So it's not untilan electric car comes along that eventually is going to have positive, withoutgetting into this argument, and let's just use it as an analogy. Most peoplewould choose an alternative if they know that it's going to be beneficial forthe environment. Let's just say that. If it's going to cost around the sameamount, it's going to do the same kind of thing or better, they'll choose thatoption.
Ramon David (00:36:36):
So saying you've got to cut out these food groups, you'vegot to cut out these food groups. You've got to stop eating this, and that'sgoing to help you is, at least I've found with the people that I've worked withover the last 20 years, is nowhere near as impactful as saying, "Removethis and replace it with this. Or just start shifting towards eating more ofthese things, and slowly start to cut some of these things out." And Ithink that most people would find that infinitely easier than just trying toeliminate, maybe for a lot of people 50% of the things that they're currentlyeating on a day-to-day basis, right?
Danny Grannick (00:37:13):
I think you're touching on one of the biggest challengeswith personalized care, which is finding a line between what the most impactfulchanges are and what the most likely changes are that a person will actuallydo. And kind of moving into lifestyle, obviously smoking is a risk factor forgum disease. Obviously you're going to get poor oral health and we cite it as arisk factor in some of these results. Do I expect every single person who getsa high gum disease risk score to quit smoking something that they may have beenaddicted to for decades based on the results of one test? No, I mean, I thinkit's infeasible and impractical to expect them to do that. So, what we can dois focus on the changes that they are willing to make in their life, and try tomitigate the risk for the choices that they're not willing to change.
Ramon David (00:38:15):
So, let's move into the oral microbiome tests, like whatthe company actually does. What's the process, what are the steps that peoplego through? What kind of information do we get, and then recommendations, howdoes it all work?
Danny Grannick (00:38:35):
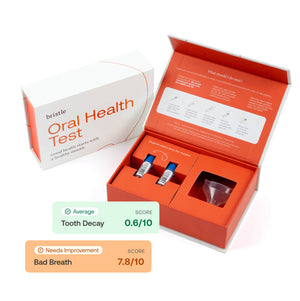
Yeah, so from a process standpoint, it's pretty simple.People just order the kit online, we're looking into distribution channels toget it into clinics and stores, but you get your saliva collection kit. Ifanybody's taken a 23andMe test before, it's kind of the same process. You goonline, you register your barcode, you fill out a short questionnaire. Ours isa bit more dental-related than what most people are used to probably, butanswer some simple questions about your clinical background, some behavioralquestions, and then you spit in a tube and send it back. We all analyze it inour lab and I can touch on the technology in a bit, but in about two weeksyou'll get your results and we just email you a link. You access them online.Right now the indications that we show, your score is related to the abundanceof bacteria broken out into indications. So, you'll see a section on your riskfor gum disease as it relates to the abundance of bacteria related to thatindication. Same thing for cavities, bad breath. And then we have a beneficialor commence kind of section as well.
Ramon David (00:39:49):
Yeah, awesome. So you touched on the tech, what's theprocess?
Danny Grannick (00:39:56):
Yeah, so this is one of the really exciting things thatwe've been working on. I guess, starting very narrowly, a lot of technologies,I kind of referenced this idea of 12 bacteria related to periodontal disease,and I think it's a good place to start. A lot of technologies today use ananalysis method called qPCR, and qPCR uses probes, so kind of like little hooksand you define exactly what you want to detect, and you're looking for thepresence or absence of that bacteria in the sample. So there are some tests onthe market that are designed to look for those 12 bacteria. And if you havethem, it'll detect them and it'll show you as high risk for periodontaldisease, which is fine. But as we discussed, most people have between a 100 to250 different kinds of bacteria in their oral microbiome, and looking for thepresence or absence of 12 seems like you're missing a lot of contextualinformation.
Danny Grannick (00:41:05):
We know that one, more than 12 bacteria are implicated inperiodontal disease. So you might have one that's not included in that test,and you'll never know if you have it. And we also know that the science behindthose bacteria is a lot more complicated than presence or absence. Some ofthese bacteria work together to drive disease. They're community-driveninfections. Some bacteria are more virulent than others. So there's a lot ofshades of gray. And in that sense, some of these Perio tests are really kind ofnarrow and missed I think a lot of positive cases. So going one step further,if you've taken a gut microbiome test, most to them use a technology called 16Ssequencing. And suppose if qPCR is like, you've got a list of 10 people, 16S iskind of like the bacterial thumbprint, you'll be able to identify all of thebacteria in the sample. So you're not restricted to a hypothesis. You can do alot of discovery efforts. But that's as far as you'll get. You'll be able toidentify what's there, you'll get some relative abundance information, andthose will be your results.
Danny Grannick (00:42:30):
The advantage there is you're getting, if you have a 100bacteria in your mouth, you'll be able to identify all 100 theoretically. Themiss is that there are other microbes in your mouth that are also implicated inhealth and disease, fungi and viruses. And that's kind of where our test comesin. So we use a method called shotgun metagenomics. And the way that our testworks is, we sequence everything in the sample. We don't make any assumptions.We don't leave anything out. We get whole genome sequence information for allof the microbes, whatever viruses we pick up, the fungi, the bacteria, and thatprovides us with a much richer dataset that we can get better insights from.
Danny Grannick (00:43:21):
So compared to 16S we're getting whole genome sequenceinformation that allows us to differentiate between different strains ofbacteria. So we can get more specific around what we're detecting and what theimplications are. We're getting micro [inaudible 00:43:36] outside of bacteria.So we can start factoring those into somebody's risk score and actually do alot of research discovery on our side. Because again, the oral microbiome hasbeen this relatively untouched area of research and the whole genome sequenceinformation also provides us with insights into functional characteristics ofthe microbes. So we can start looking at how different microbes work to get todrive disease, which can inform potentially new therapeutic targets andinterventions in the future.
Ramon David (00:44:09):
So we take the test, we implement some of the recommendations.So we have the intervention, and then we retest after a period of time. Isthere a recommendation for how often we do this, or how many times a year we dothis?
Danny Grannick (00:44:26):
Yeah. So right, we're actively doing some research aroundwhat the optimal cadence is. I think it'll differentiate from person to person.We have a single test option, and then we have a twice yearly and quarterlysubscription option. But we think that monthly is actually going to be the mostimpactful kind of cadence to measure your oral microbiome. I think for certainpeople, there's a lot of different use cases for why people are taking thetest. I think there's people that want to use this as ... There's people thathaven't been to the dentist in a few years and want to use this as, for lack ofa better word, a gut check on their oral health. So, that's kind to where thesingle test comes into play. But the majority of our users are actually, andit's a sad term, but we have deemed them as frustrated sufferers, which I thinkprobably resonates with a lot of listeners.
Danny Grannick (00:45:32):
These are people that have been, like my co-founderbattling oral disease their entire life, and have been trying to do theseinterventions or get a more specific diagnosis and haven't been able to getinsights. It's this recurring cycle of procedure, very invasive, expensiveprocedures, a waiting period, kind of anticipatory nightmare of when your nextdental appointment is. And then you rinse and repeat. And this is kind of wherethe test starts to evolve more into what I would call chronic diseasemanagement than anything else. These people are getting an accurateunderstanding of what the bacterial drivers are at their condition. They'reable to test a bunch of interventions and see which ones work the best. Andbecause our test detects those pathogenic bacteria at the very smallestamounts, a lot of the times we can detect risk for disease before thosephysical symptoms have manifested.
Ramon David (00:46:36):
Right. Can you share with us a case study and maybe useyour co-founder, who's Brian, right?
Danny Grannick (00:46:44):
Yeah. Yeah.
Ramon David (00:46:46):
I don't know if you want to use him as a case study, but-
Danny Grannick (00:46:48):
Oh, no. I love using him as a case study.
Ramon David (00:46:50):
Maybe share with us some of the insights that have comeout of the test, some of the recommendations that have been implemented, andthen what kind of changes have been found?
Danny Grannick (00:47:02):
Yeah. So, I'll use, I guess for background, we've beendoing a clinical research study with the University of the Pacific dentalschool, amazing team of clinicians and students in San Francisco. And we'vebeen analyzing patient samples and then getting access to electronic healthrecords and the dental diagnosis from that day. So that's provided us with thisamazing kind of clinical baseline that we can use for characterizing oraldisease. In a few of those cases and what we've seen with our users is,patients will go into the clinic for a checkup and they'll be diagnosed ashealthy. And we will actually be able to detect a significantly high abundanceof cavities causing bacteria let's say. Now, they didn't have signs of decaywhen they were in the clinic. So they weren't, nothing showed up on an x-ray orthey weren't even x-rayed in the first place, because the dentist didn't seeanything.
Danny Grannick (00:48:05):
But according to our test there's a really high abundance.And for better or for worse, one of the best interventions that you can do is ahigh fluoride prescription toothpaste for obviously a limited amount of time,but it helps strengthen the enamel and prevents the onset of decay. So we'vehad cases where users have detected high abundances of cavities causingbacteria, even within weeks of a dental appointment that was missed, and havetaken on interventions and lowered the abundance of that bacteria. So somethingthat theoretically could have progressed into a cavity and probably a fillingor a root canal or something like that at their next six month checkup ismitigated now.
Ramon David (00:48:57):
Yeah, that's-
Danny Grannick (00:48:59):
And I think there have been some other, we've started tosee a lot of, well exciting and tragic edge cases that I think speak to thisidea that oral health is a lot more than cavities or gum disease. So like Isaid, usually people have between a 100, 250 different kinds of bacteria intheir mouth. There's a lot of diversity and it's the balance of those good andbad microbes that determines your risk for oral disease. But we've started tosee some cases come through where they didn't have any bacteria related to oraldisease. So they didn't have those red or orange complex bacteria when they gottheir results back. For all intents and purposes, their risk was low becausethey didn't have the bacteria that cause or were related to cavities and gumdisease.
Danny Grannick (00:49:54):
But what we did find was, some of these patients only hadfive or six bacteria that made up the entire oral microbiome, and that's it. Soit was this extremely low diversity. And in a lot of those cases there was onedominant bacteria that made up 80 to 90% of the oral microbiome. And in thosecases we've actually started to see some consistency in what that bacteria was.So it's a bacteria that is traditionally found on bathroom tile. I don't knowif you've ever been in a bathroom and seen like this pink or orange kind of huein grout maybe, but it's that bacteria and it's an opportunistic pathogen. Sothe way that that works is, it won't be harmful in the oral cavity, but what itwill do is, if there's an opportunity for it to land, it'll then expand fromthere and kind of take over whatever it's in. Now, it's not pathogenic. So someof these patients had no symptoms of oral disease. They took the test out ofinterest or for whatever reason, but we uncovered this really big anomaly withtheir results.
Danny Grannick (00:51:14):
And while this bacteria isn't pathogenic in the oralcavity, it is extremely pathogenic if it makes its way into the body. Thisbacteria, one of the bacteria that we found I think was tied to one and a halfpercent of hospital acquired infections in the United States, causes severerespiratory infection. And these patients, we're digging through the data andthis is going to be an ongoing kind of internal research study. But we havestarted to see associations between certain medications and this anomaly andthe results, specifically with patients that are taking immunosuppressants orpatients that have taken courses of antibiotics in the past.
Ramon David (00:51:59):
Do we know if this is picked up from places likebathrooms?
Danny Grannick (00:52:05):
Yeah, so we need to validate exactly where bacteria areoriginating. My unproven, take it with a grain of salt answer is, I think a lotof people put their toothbrushes directly on the sink or in the bathtub, likeon the rail of the bathtub. And my guess is that that was the path ofintroduction for this bacteria into the oral cavity. And I think it's a mixtureof that in the fact that very few people replace their toothbrushes as often asyou should replace your toothbrush.
Ramon David (00:52:44):
How often?
Danny Grannick (00:52:44):
For everybody listening,
Ramon David (00:52:48):
Do you have regular-
Danny Grannick (00:52:51):
There was a study. I mean, I think replacing your toothbrushevery, I think the last recommendation I saw was every three or four weeks.
Ramon David (00:52:59):
Oh, wow.
Danny Grannick (00:53:00):
Yeah, it's pretty often, I would say more often if you putit on your sink. Or maybe just buy a toothbrush holder.
Ramon David (00:53:12):
Yeah. Is the oral microbiome much like the gut microbiomein the way that we want more diversity? It's beneficial to have the diversity?
Danny Grannick (00:53:26):
The jury's out on them. There hasn't been enough research.There's been very little research looking at the connection between diversityand oral health. I think initial studies have actually shown the opposite, thatslightly lower diversity is tied to better oral health. But the studies areextremely small populations. They most likely used qPCR 16S which for us isn'tkind of meeting the standard. So, that's another thing that we want to lookinto. And it's an advantage of our platform is that as more people take thetest, we'll be able to lead and disseminate a lot of these discoveries.
Ramon David (00:54:08):
What's the future for this space? What do you see in 10years, or what do you hope for in say 10, 20 years time?
Danny Grannick (00:54:16):
I would like to see the same thing that we're seeing inevery other area of healthcare. And I think the unfortunate thing is, oralhealth has just been the last person to the party. With infections and the gutmicrobiome, we're moving towards this idea of precision diagnostics, precisionmedicine, personalized care. And we're trying to do the same thing with oralhealth. I think there's some parallels with oncology as well. We're starting tomove into liquid biopsies, which is being able to detect DNA that is shed fromthe earliest signs of a tumor. So these mutated strands of DNA in a bloodsample. And by detecting cancer earlier, we can intervene sooner and have shownthat that drastically improved outcomes on the other side.
Danny Grannick (00:55:12):
There's no reason to me why we can't take the sameapproach with oral health. Our test detects the bacteria related to thesediseases at the very smallest amounts before these physical symptoms haveemerged. And when you detect disease that early, you can intervene sooner andimprove outcomes on the other side. So I think that's kind of the first big legis, shift this reactive symptoms first approach to oral health to one that'sprevention focused. The second leg, and I think we're seeing this in other areasof healthcare as well, is getting a lot more specific around how we diagnosedisease. Alzheimer's is actually a really good example. So, there's a lot ofareas in health where we have traditionally diagnosed disease from asymptoms-first approach. And I think Alzheimer's is one of those things whereit is to me kind of an umbrella term, right? We haven't necessarily tied typesof Alzheimer's to specific causes yet, but we're kind of moving in thatdirection.
Danny Grannick (00:56:17):
And oral disease is kind of the same thing. Two people canhave gum disease, periodontal disease, but that periodontal disease can bedriven by completely different bacteria. And based on what bacteria is drivingyour condition, it may lead to one intervention being more effective thananother. So, that's kind of the second leg is moving our idea of diagnosingdisease into a much more precise characterization based on molecular analysisrather than symptoms-based analysis. And then the third piece is really provingthat improving oral health can improve overall health outcomes. I would love tosee us kind of lead the charge showing that reducing certain pathogenicbacteria in the oral microbiome reduces the rate of heart disease, or can helppeople better manage diabetes or reduce the rate of cognitive decline.
Ramon David (00:57:16):
Yeah, super cool. I just love where this is all going.It's very, very exciting. A very, very exciting time I think this, the lastmaybe decade leading up to the things that have been happening and everythingthat's going on now, what's going to happen over the next 10, 20 years. Verycool.
Danny Grannick (00:57:36):
Yeah, it's been amazing. I mean, I think, seeingtechnology's like an Oura Ring that can measure your sleep, it's a really goodanalogy. You wake up in the morning and before you had an ability to measureyour sleep and understand what good sleep meant. Because, "Man, I feellike shit. I had a bad night of sleep. I guess I should go to bed earlier, or Idon't know." And now that we can measure it, I think we can, it opens upthe ability to understand and improve at a scale that I think we just neverbeen able to do.
Ramon David (00:58:14):
Yep, yep. I love it. I'm constantly running tests. Infact, some of the very first tests that I did were with the second gen OuraRing and I did single case study design for myself for CBD oil for sleep, forcertain peptides, GH-releasing peptides, different types of magnesium, likethese sorts of things. And you see the impact, was it probably about threenights ago, just started another three month block of CJC-1295, and [inaudible00:58:53] peptides. And my deep sleep goes from around 10, 11% to 18 to 20%overnight. Like it's just, and the trends stay that way just because of thesepeptides.
Danny Grannick (00:59:05):
And that's, I think that it goes back to your commentaround dietary changes. It's like everybody can stop eating sugar and kind oftake that as a net benefit. But I think that cutting out sugar may drasticallyimprove outcomes for a certain type of person, like in a certain population andmaybe not be as beneficial for another. And there should be another changethat's introduced to those people. But we will never know if we can't measure-
Ramon David (00:59:35):
Exactly.
Danny Grannick (00:59:36):
... those changes and the outcomes and that's really kindof the goal with Bristle.
Ramon David (00:59:41):
Yeah, exactly. I love that, because as you say, withbiochemical individuality, you just don't know, unless you can measure it andtest it and look at the trends and everything. How do you even know when youcan go off the subjective report, like I feel better and that might be okaywith something like getting a good night's sleep, but there's no feeling betteraround the impact of the things that we're doing is going to have three monthstime from now, a year from now. The impact that it has on reducing thelikelihood of certain cancers or dementia or things that are going to impact usin decades from now, right? There's no feeling around that. Oh yeah, I feellike this thing that I'm doing is going to help me not get cancer in 30 years.
Danny Grannick (01:00:24):
And I think it would be like, I think the other excitingthing here is that a lot of the interventions that we're uncovering aren't themost expensive and invasive and therapeutically complex options. It's not, theinsights that we're getting on, we need to go develop this billion dollar drugand bring it to market. It's look at how a simple change in behavior or diet orlifestyle can have massive impacts on your overall health outcomes. And it'sall because we can quantify it finally.
Ramon David (01:01:03):
Yeah, yeah. That's a really great point. And I don't wantto give our listeners, and I've said this before the, I don't want to implantthis idea that you need to start going out and start taking peptides and doingall these sorts of crazy biohacking stuff. Simple, simple things can have amassive impact, like with sleep. Generally going to bed at the same time,getting up at the same time in the morning, getting some sunlight to set thatcircadian cycle and making that regular is going to hugely impact the qualityof sleep. There's so many free and cheap things that we can be doing that havea really big impact.
Danny Grannick (01:01:44):
Yeah. I mean, for my sleep, being able to kind of finetune and say, "Not only do I feel better in the morning when I go to bedbetween 09:00 and 9:30." I can measure exactly the change and how and whyI feel better. And that I think is the difference between implementing andreally adhering to a lifestyle change and just kind of noting it in your headand then completely forgetting about it the next day. And it's the repeatedadherence to those changes, that's going to drive better outcomes. It's notthis one off, "Oh, I feel a little bit better this morning. I'm going togo out until 2:00 AM tomorrow night."
Ramon David (01:02:30):
Yep, exactly. Danny, this has been a great chat. Love whatyou guys are doing. Can't wait to see more. Where do people go to learn moreabout Bristle Health?
Danny Grannick (01:02:43):
We are publishing content all the time. I would recommendeverybody visit bristlehealth.com. We've got a bunch of blog articles, a lot moreon the way. I think people have been surprised about just how much informationthere is, and I think it's a great learning experience.
Ramon David (01:03:02):
Love it. Awesome. Thanks very much for being on the show,man. Appreciate it.
Danny Grannick (01:03:05):
Thanks for having me, yeah.
Ramon David (01:03:05):
That's it for this episode. If you want to support theshow, make sure to subscribe on Apple Podcasts, drop a five star review orfollow us on Spotify. And guys, make sure to head over to mybrainfirst.com tocheck out the latest resources and products to help you upgrade your brain andlife. Thanks for tuning in. Talk to you soon.