What effect does mouthwash have on the oral microbiome?
This really depends on the type of mouthwash. Many of them non-specifically kill microbes and reduce the overall microbial load in the mouth. This slash and burn approach that we’ve generally used for decades has a generally negative effect on the oral microbiome and came about before we had a better understanding of how the existing microbiome is important for preventing disease. In one example, a study showed that chlorhexidine mouthwash can result in relatively dramatic (and negative) shifts in the community. Depending on what is currently in your oral microbiome, the slash-and-burn approach might be beneficial for you, but possibly detrimental as well.
Do you have any recommendations for fresh smelling breath that won't wreck our biome?
Studies have found tongue scraping and certain mouthwashes (those containing cetylpyridinium chloride, and sodium chlorite) may reduce the levels of these species without harming the beneficial microbes.
How does kissing someone impact each other's oral microbiome?
Great question! Intimate kissing (unfortunately) has been shown to impact the oral microbiome. Partners have been found to have more similar oral microbiomes than non-relatives. In a study of 21 couples, an intimate kiss did not lead to a significant additional increase of the average similarity of the oral microbiota between partners. However, clear correlations were observed between the similarity indices of the salivary microbiota of couples and self-reported kiss frequencies, and the reported time passed after the latest kiss. Bacteria transferred include those that have been shown to cause cavities and gum disease - so make sure your partner is brushing and flossing 😊
Probably should have done this AMA before Valentine's Day... my bad.
Source: [https://microbiomejournal.biomedcentral.com/articles/10.1186/2049-2618-2-41](https://microbiomejournal.biomedcentral.com/articles/10.1186/2049-2618-2-41]()
Might the similarity in couples' biomes be connected to the couples similar eating habits as in often eating the same food (especially the ones living together)?
It's a great point! Diet likely accounts for some degree of the similarity. In the referenced study, though "by far most pronounced similarity for communities associated with the tongue surface" - which for the purpose of the study likely was explained by kissing frequency.
How big of an impact do tonsils have on your oral microbiome? Do they help or hinder the development of healthy flora? Similarly how dangerous are tonsil stones to your oral health?
Great question! A few studies have attempted to address this relationship. However, I believe the jury is still out on how tonsils affect the microbiome, and vice versa. There is certainly a relationship between tonsils and the microbiome, but what that is exactly is unclear. Sorry for the unsatisfactory response! Maybe we'll launch a study to investigate this more directly!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5774679/
https://journals.asm.org/doi/10.1128/mSystems.01302-20
https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-019-0956-5
https://www.nature.com/articles/s12276-020-00487-6
I get canker sores a lot. Less now that I'm an adult, but if I bite my cheek, it's pretty much a given. Any ideas why? There's not enough research on it and it drives me nuts.
Some studies have pointed to a correlation between specific oral pathogens and titers of HSV-1 (causative agent of cold sores). Any number of molecules (including those released via inflammation) may be involved in reactivation of latent viruses such as HSV-1, which can result in the presentation of a cold sore.
At Bristle we haven't specifically looked into changes in the oral microbiome prior to or during canker sores, but I believe it would reveal some interesting findings that may help reduce those triggers.
https://pubmed.ncbi.nlm.nih.gov/23611298/
https://pubmed.ncbi.nlm.nih.gov/17804655/
How does eating blue moldy cheese effects? Are these molds considered good?
Some molds can potentially be beneficial to the oral microbiome but like anything else, it depends on what kind of mold we're talking about. What you might be referring to is some research showing that eating cheese can reduce risk for cavities. Cheese includes a few proteins - namely casein - that help reduce enamel demineralization. It's also thought the increased salivary flow from eating cheese helps keep your teeth clean.
I'd stay away from old moldy cheese though tbh... or eat a bunch then take our test :)
How do things like teeth-whitening strips, charcoal toothpaste, and other whitening products have an effect on the oral microbiome?
Lots of products touted as "beneficial" aren't. We often mistake good oral health for being a bright smile, minty breath, and straight teeth. Many whitening products are great for aesthetics but wreak havoc on your oral microbiome and can cause a variety of oral conditions down the road.
Is oral microbiome related to gut microbiome? Are there ways to improve oral flora, similar to how eating fermented foods can help diversify gut flora?
Yes! The oral microbiome is closely linked to the gut microbiome. Some studies have shown associations between IBD, Crohn's disease, and even colorectal cancer with bacteria in the oral microbiome. Here are two recent reviews on the oral-gut axis.
https://pubmed.ncbi.nlm.nih.gov/33924899/
https://www.frontiersin.org/articles/10.3389/fimmu.2021.620124/full
Are there any “good” microbes in the oral microbiome like there is in the gut flora?
Yes, there are indeed "good" microbes in your oral microbiome that prevent pathogenic microbes from invading the space. Their abundance is strongly associated with good oral health and similar to gut microbes and gut health.
Is there a way to promote the good bacteria? And do traditional mouthwashes with alcohol/hydrogen peroxide hurt the good part of the microbiome?
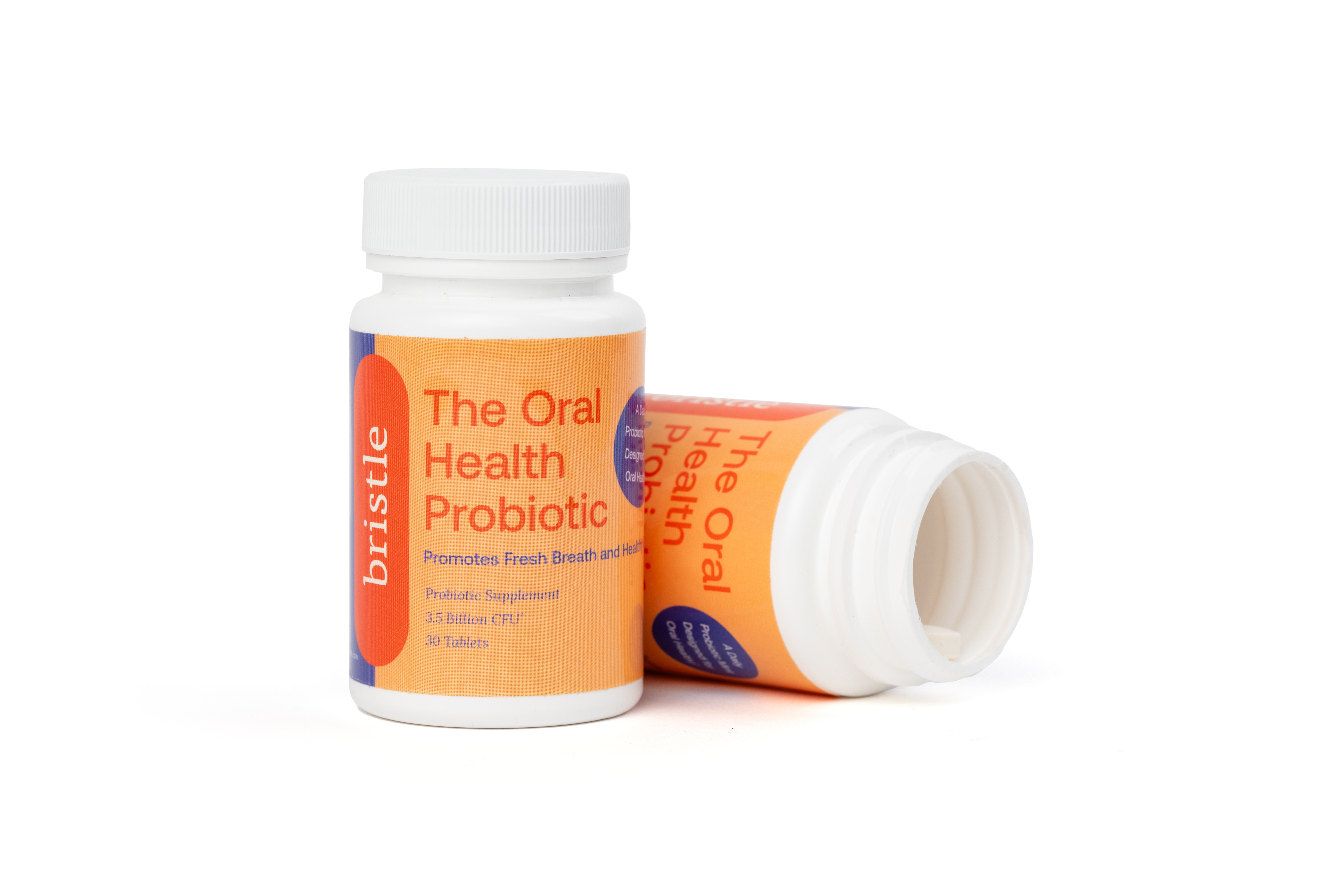
Yes, indeed there are ways to promote the growth of good bacteria including changes to diet, lifestyle, and taking some products. Yes, traditional mouthwashes have been shown to indiscriminately kill "good" microbes and "bad" microbes alike. There are a few oral probiotics on the market that may have some clinical efficacy, but this depends on your existing oral microbiome, as more of a good thing doesn't necessarily make it better.
What else are you going to do with the data? Will it be made available to law enforcement? Other researchers? Commercial development? Insurance companies?
Data privacy is a top priority for us. We give you choices to control how your personal information is used, stored, or shared. We will never share your data without your consent, and will only ever do so in the name of advancing oral health research or your request.
We will use the data to advance research on the oral microbiome and oral health. This includes measuring how different interventions (oral care products, diet, etc.) impact the oral microbiome at the species level, so we can give personalized insights into how to promote good bacteria while eliminating just the bad - and ultimately developing more targeted and effective therapies/treatments. We also use aggregate, de-ID'd data for uncovering new biomarkers from the oral microbiome, which turn into new features for our users.
You own your personal data and control access to your results, so we can't "sell it" to companies. Insurance companies don't reimburse for our test which means we have no conflicting duties to provide them with your data (and can't anyway without your consent). In the future, I can imagine insurance companies being interested in accessing your data for better ("You have great oral health! Here's a lower premium.") or for worse ("You haven't been taking care of your oral health, and your rates may increase."). Honestly, we've barely scratched the surface with insurance given how novel our test is and how overlooked oral health has been. Ultimately, there are laws protecting your genomic data from being used by insurers to change your rates and I would assume something similar for our test - so you would (ideally) only benefit by getting rewarded for improving.
You can learn more about the steps we take for ensuring your privacy on our site. Let us know if you have any questions!
What exactly causes halitosis? What creates the awful smell?
There are a few different categories of halitosis. However, 90% of halitosis cases come from intra-oral halitosis, which is caused by the production of volatile sulfur compounds (VSCs). VSCs are the same compounds released by rotten eggs that give them their distinct odor. Bacteria in your mouth are capable of producing VSCs. Bacteria that coat your tongue and reside at your gum line have been shown to produce VSCs.
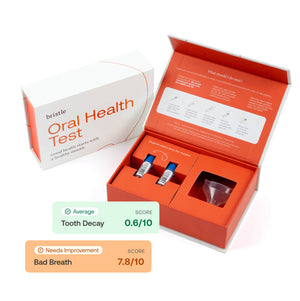
You can use Bristle to find out which of these microbes is in your mouth and how you can address them.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7342603/
Are you guys doing 16s or shotgun? Technical bias could potentially be introduced just by having different library prep methods (ligation vs tagmentation have their own gc biases) or even different collection methods (swabs, saliva, etc). Do you guys observe that? Are you guys classifying to known bacteria or are you also going to try to look at unknown things?
Great questions, we use shotgun for improved resolution over 16s. We attempt to relieve some of the technical bias through automation. I won't go into details about our library prep method, but I can say we've done extensive testing to demonstrate consistent detection (of specific microbes) across samples (and time). We are focused on saliva for a number of reasons, one of them being consistency. We find it difficult to get a comprehensive view of an oral microbiome using a swab, which would rely on users swabbing an area and not contaminating it with skin or other microbiome.
The challenge of the unknown is that much of the nucleic acid in saliva has no matching reference genome, so its annotation is nearly impossible. However, we do work on the "known unknown" which is things that are mappable but also distinct from reference genomes, which gives Bristle a unique metagenomic database to work from.
Why do some people who take very poor care of their teeth have zero cavities, while others who are extremely vigilant have major problems? Is it genetics? Luck? Is it related to the microbiome?
Great question! This phenomenon was actually one of the reasons we created Bristle. I have too many cavities to count despite doing my best hygiene and was told I have "bad teeth", which was an insufficient explanation in my opinion. There are a number of factors that influence cavities, such as genetics (enamel strength, sugar metabolism), diet, dry mouth/mouth breathing at night, and teeth grinding - but the oral microbiome can play a major role. In testing mine, I found I have a higher abundance of cavity-causing bacteria, so I've started chewing xylitol gum and taking other steps to reduce them! We have more information in our blog here: Are some people more prone to cavities?
Microbiome testing companies have a shady past. What are you doing to ensure you're following the science and not the marketing and pop science?
A core value of ours is to let the science and literature be our guide. The oral care space (like much of healthcare) is filled with products claiming benefits but not being backed up by evidence. We created Bristle as a way to measure the impact of these products and other interventions (diet, lifestyle) so patients can make more informed decisions for their health. We believe transparency is one of the biggest ways we can help our users. We don’t have all of the answers, as the data is still sparse, but our goal is to equip users with information on what we do know so they can find what works best for them. I’m someone who has suffered from oral disease my whole life (too many cavities to count) and I’m determined to help build the future where others won’t have to.
Do you provide actionable insights and make recommendations? What percentage of your findings end in “talk to your doctor?”
We do! Our recommendations include ingredients/products, diet, lifestyle, and hygiene recommendations to improve oral health.
Not many of our findings end with "talk to a doctor." I think this has been a huge problem with at-home testing - not having an effective way to close the loop on behalf of the patient. While we encourage our users to share & discuss their results, our primary focus is providing insights and actionable recommendations to improve oral health directly to our users.
Some of our users have existing & severe oral disease, in which case they are already working with a provider (usually). There's clear value in understanding the oral microbiome and oral health status as a monitoring tool. Other users are fine and just want insights into their oral health, or have early symptoms and want to know what's going on. Our goal is to help people manage their oral health and prevent disease, so ending our report with "talk to a doctor" wouldn't be super impactful and I doubt people would act on it.
A couple of other pieces:
The oral microbiome is still in the earliest stages of being adopted to the standard of care, so it's likely that a provider wouldn't get much further than you (our results are easy to understand). Additionally, only 50% of US adults even see a dentist every year, so referring folks to a dentist as the only next step doesn't really help if they never go anyway.
Our focus is helping our users understand and improve their oral health on their terms - whether that's with or without a provider. Of course, we do encourage everyone see their dentist & physician regularly regardless :)
Do you make recommendations for prescription or OTC products, and if so, do you provide for this and manage medication interactions?
Most of our recommendations will be for OTC products. We do not sell any ourselves, but instead, link out to some products that contain the ingredients we recommend and come well recommended by the dental provider community. For medication interactions, we encourage users to consult with their physician to see if there are any concerns.
What education do you provide about these products to clinicians as part of your product offering? And what training do you provide your service representatives in counseling users in how to interpret results?
Our recommendations focus on the ingredients, with an explanation of what research has shown their benefits to be (lowering mouth's acidity, remineralizing enamel, destroying cavity-causing bacteria). We believe it's more important to educate consumers on the why behind our recommendations rather than just giving them a list of products.
I can't comment on the Promethease situation. I will say we've designed our report to be interpreted by a layperson and are conscious of how we present results for this kind of concern. I think 23andMe has done a great job of setting the example for how to present information to properly educate users on risk.
In my opinion, it would be an imbalance of certain species associated with oral conditions.
How much does your own genetics actually effect your propensity to develop mouth diseases like periodontal disease, tooth decay, bad mouth biome, etc?
Studies have found that genetics can play a role in the propensity to oral conditions, particularly in factors like your immune response to infection, sugar metabolism, and dental enamel. I was told I have genetically bad teeth, so I'm quite familiar :)
Our hope is that by better understanding the oral microbiome we can better understand these propensities, and develop more effective care plans based on each individual's oral microbiome/health.
We cover this a bit more in our blogs on Are some people more prone to cavities? and Is gum disease contagious?
Is the oral microbiome similar to our sinus microbiome, as they're touching? Will you branch out if successful into testing sinus or gut microbiomes?
The oral microbiome is itself already incredibly diverse, with bacteria that colonize your tongue being different from those on the roof of your mouth or those on your gums. This means that each niche is unique by comparison to the sinus microbiome.
We are focused on the oral microbiome because it is accessible, can be modulated, and most importantly, changes to the oral microbiome may prevent the onset of irreversible disease. For example, for decades we've known about bacteria in the mouth that cause expensive and irreversible periodontal disease, and by addressing these microbes we can prevent disease from happening.
Would it be (at least theorethically) possible to make (or modify) some sort of bacteria to "add" to your oral biome, to outcompete the bacteria causing bad things, and not be bad for us themselves? Like a cooperation where we would feed them (by feeding ourselves) and they in exchange would protect our mouths?
Yes! The two things you're describing are bucketed into "probiotics" and "prebiotics"
Probiotics are beneficial bacteria. The intent is to introduce them to your oral microbiome so they can outcompete pathogenic bacteria residing in your mouth. We include recommendations around these as part of our results.
Prebiotics include foods or supplements you take that "feed" the probiotic bacteria to increase their relative abundance and therefore their beneficial effects.
You can also make changes that reduce the abundance of pathogenic bacteria. An easy example is reducing sugar intake if you have a lot of cavities-causing bacteria. These bacteria feed on sugar and produce acid as a byproduct, which decays the enamel on your tooth and eventually the tooth itself. By reducing sugar intake you restrict the "fuel" these bacteria need and can lower their levels over time.
Our mouths are home to plenty of beneficial bacteria. It's the imbalance of beneficial to pathogenic bacteria that drives oral disease!
Is there any research into the effects on the oral microbiome from yeasty alcoholic drinks like beer vs spirits?
We haven't compared the differences between alcoholic drinks, but a study from NYU found that "compared to nondrinkers, men and women who had one or more alcoholic drinks per day had an overabundance of oral bacteria linked to gum disease, some cancers, and heart disease. By contrast, drinkers had fewer bacteria known to check the growth of other, harmful germs."
What current flaw in oral microbiome needs to be changed?
I think the biggest flaw is that the oral microbiome isn't addressed as a component of oral health/dental care! Decades of research have established causal links between bacteria in our mouths a some of the most prevalent oral diseases on the planet including cavities & gum disease. We have the tools to measure the oral microbiome but it hasn't been adopted as part of the standard of care.
There are some barriers here - misaligned incentives between stakeholders, education for providers & patients, etc. but they are all solvable problems that we're tackling at Bristle.
If we can get everyone leveraging the oral microbiome as a standard of care we will see improved outcomes - the lift is spreading awareness & education about the oral microbiome and creating a model that incentivizes using it.
Broadly wrt microbiome testing - companies tend to use outdated methods like qPCR or 16s that miss a lot of important information contained in your microbiome. More companies should invest in better technology for their tests!
One more thing: Nearly half of US adults have a form of gum disease and over 90% have cavities, and both are largely driven by an imbalance of the oral microbiome. Additionally, research has been unveiling links between oral health and the risk or presence of systemic diseases, including diabetes, heart disease, and Alzheimer’s. One of the more exciting things we'll be able to do as we grow our database is looking for oral microbiome signatures related to other diseases, in hopes of discovering more effective therapies and interventions.
Do you see a future where microbiome be used as a unique identifier of persons? If so, how long can a sample be viable for and what methods could be used to preserve a record?
I personally don't see a situation where the microbiome is used for ID purposes - at least in the near term. The oral microbiome is a pretty dynamic environment to the point where it would be difficult to pair a profile with an individual, unlike something static like your DNA. There are so many things that can affect your oral microbiome profile - products, diet, hygiene, etc. It would be pretty easy to cause a shift in what your oral microbiome looks like.
That said, there have been some studies showing similarities in oral microbiome profiles between partners and parents/children - so it's possible to have something like a "familial" oral microbiome profile, but not to the extent you're describing.
Can bad oral health influence mental wellbeing?
Absolutely! The oral microbiome (and oral disease) has been implicated in a number of neurological disorders. The most well known example of this is the relationship between periodontal disease and Alzheimer's disease. https://pubmed.ncbi.nlm.nih.gov/32280099/. Strikingly, antigens from periodontal pathogens can be found in the brains of patients with Alzheimer's disease. https://pubmed.ncbi.nlm.nih.gov/34720846/
Additionally, migraines are associated with the oral microbiome (which is in part responsible for nitrate reduction, an important regulator of vasodilation).
The oral microbiome (similar to the gut microbiome decades ago) likely plays a role beyond what we know so far, and can impact cognitive functions in ways we don't yet understand.
The comments here sum it up - oral health can influence mental well-being on the psychological and physiological level.
We put way too much emphasis on white, straight teeth and not enough on good oral health. Unfortunately, lots of people become embarrassed by their mouths and lose the confidence to express themselves. It's tragic. Sometimes it's just bad breath, other times it's severe oral disease that goes untreated because people can't get the care they need.
There are also some interesting studies associating oral health with mental health - connections have been made between oral health & headaches + cognitive decline + depression.
Can you talk about fluoride? Is it bad for our oral microbiome? What is a good alternative?
Research has found fluoride prevents and treats dental cavities by promoting favorable remineralization of the tooth enamel while concomitantly impairing bacterial metabolism. Research into the drawbacks of excessive fluoride is still ongoing, so we encourage users to decide what makes the most sense for them. A great alternative is nano-hydroxyapetite, which has shown similar benefits to fluoride. Another ingredient to consider is Xylitol, which has shown some promise in reducing the levels of cavity-causing species.
How can I as a vegan best take care of my teeth? I know that long term carbohydrate consumption can damage them and I'd like to keep my chompers!
Great question! Proper oral hygiene will be the most effective thing you can do to keep your chompers healthy. On the diet side, you are correct that carbohydrate/sugar consumption can lead to a harmful oral microbiome (more acidic). We cover beneficial foods more in-depth in our blog here, but to summarize:
Ultimately the best way is to stay on top of your oral health, which our test can help with (sorry for the shameless plug)!
Does probiotic mouthwash and toothpaste help with bad breath? I've had issues with gut health that has affected my breath. Probiotics help (fermented foods and pills), so I'm wondering if probiotic oral products do too.
Studies have found tongue scraping and certain mouthwashes (those containing cetylpyridinium chloride, and sodium chlorite) may reduce the levels of these species without harming the beneficial microbes. We're still looking into probiotics, but Streptococcus salivarius strain K12 (usually just called K12) has some data supporting its use.
Glad to hear probiotics have worked for you!
Shameless plug: Our test can give you a breakdown of the levels of sulfur compound-producing bacteria in your mouth to see if they are the cause of bad breath!
I have Sjogrens and am obviously concerned about how it affects my dental health, body, etc. Its not a well known disease, so there doesn't seem to be a lot of options for us. I have horrible dry mouth, lose my voice quite often and am basically told - drink plenty of water, take your MTX, HCQ and Pilocarpine when Flaring. Will there be a time when oral biome research goes beyond just informing us we have a low level of microbiota as our dry mouth is inhospitable?
Thank you for your question and I’m sorry to hear about your issues with Sjogrens. We have a lot of users in the same boat and I agree that Sjorgen’s does not get the attention it needs.In some ways, our test is already beyond just telling you that you have a “low level of bacteria.” We will report all of the species of bacteria in your oral microbiome and their relative abundance (the amount of each). Some of these bacteria are pathogenic and related to disease, while others are beneficial to oral health. In this sense, we can already provide insights beyond the bacterial levels - giving you the actual makeup of your oral microbiome and how those microbes are related to various conditions. Dry mouth is a common symptom of Sjorgens, but it's also relevant to know whether it is actually increasing the abundance of bacteria related to cavities. If it's not, then it's hopefully one less thing you have to worry about.As we build our database, we will get to the point where we can measure how different interventions (oral care products, diet, etc.) impact the oral microbiome at the species level, so we can give personalized insights into how to promote good bacteria while eliminating just the bad.Additionally, we hope to uncover new biomarkers in the oral microbiome related to conditions outside of the mouth. Our mouths are gateways to our bodies - letting in potentially pathogenic bacteria that cause other issues - and mirrors of our health - with oral microbiome shifts signaling other issues that may be happening in your body.
What are some inexpensive solutions a person could use to mitigate the negative impacts of a high carb diet on their microbiome?
One inexpensive solution is to start chewing sugar-free or xylitol gum after you eat. This will help stimulate saliva production which can neutralize the pH in your mouth and wash away excess sugars. Xylitol has additional benefits of reducing cavity-causing bacteria.
Your website states that only 50% of Americans regularly go to the dentist for check-ups. Are you trying to target that market or the market for those that don’t attend regular check-ups? If people already aren’t going for reactionary care, why would they purchase preventative care?
The top three reasons cited for not getting dental care are cost, inconvenience, and anxiety! People don't go because they don't care, they don't go because there are financial, physical, and mental barriers based on the (reactionary) standard of care today. Unfortunately, this avoidance results in the high prevalence of oral disease we see today, which end up becoming emergencies that require extremely invasive & expensive procedures. Most people are avoiding consistent care and end up needing emergency care. Bristle helps solve those three problems 1) preventing disease is less expensive than treating it, 2) we ship our kit directly to users and they access results/recs online, 3) it's just a saliva sample :) no needles or drills required - and hopefully never will be.
All that said, we are not a replacement for dental care. More dental care doesn't necessarily mean better oral health, but maintaining good oral health almost certainly means less dental care.
What does a rinse like Chlorohexadine Gluconate do to your biome? Any thing one should do after using this rinse to restore healthy oral biome?
A few studies have indicated that Chlorhexidine gluconate can negatively impact the oral microbiome by dramatically shifting the community. https://www.nature.com/articles/s41598-020-61912-4
this study demonstrates that mouthwash containing CHX is associated with a major shift in the salivary microbiome, leading to more acidic conditions and lower nitrite availability in healthy individuals.
In summary, we don't advocate for a slash-and-burn approach of antibiotics because repopulating the slash-and-burned microbiome is challenging, similar to in the gut microbiome. A few oral probiotics exist that can assist in oral microbiome reconstitution, but they may not always be effective.
Is it correct that reducing carbs in diet and increasing fibers positively affects mouth microbiome?
You are correct that carbohydrate/sugar consumption can lead to a harmful oral microbiome (more acidic), and vegetables high in fiber have been shown to stimulate saliva production and neutralize acid, both of which protect teeth from decay. They also tend to be high in vitamins A and C, which aid in rebuilding tooth enamel and helping gums heal quickly from wounds, respectively.
We cover more beneficial foods more in-depth in our blog here!
Why are your hands so big?
You can ask my lawyer