Do your gums bleed whenever you brush and floss? It may seem normal, but bleeding gums are often a sign of poor oral health. For many people, bleeding gums have become the norm after their regular hygiene routine of brushing and flossing. What you may not know is that bleeding gums are actually a sign of a bacterial infection that causes gum inflammation called gingivitis.
Bleeding gums and the oral microbiome
Bleeding gums are usually a sign of gingivitis, which is usually caused by specific bacteria in your mouth that live at the gum-line and cause inflammation. Some bacteria, such as Porphyromonas gingivalis and Tannerella forsythia, are highly adept at causing inflammation, and can evade the immune system while invading your gum tissues. We call these bacteria subgingival or periodontal pathogens. Some other bacteria do the opposite, and can actually help to prevent the pathogenic species from invading, and also help to train your immune system against these pathogens. We call these bacteria commensals or symbiotic bacteria due to their helpful nature.
Now on to the reasons your gums bleed and what you can do about it.
1. Oral microbiome dysbiosis
Some people never have bleeding gums despite never flossing, and some people get bleeding gums all the time! Genetics may play a small role in progression of gingivitis, but for the majority of people, oral microbiome imbalance is the cause of bleeding gums. Your oral microbiome hosts bacteria, fungi, and viruses that work symbiotically with you to normally prevent infection. However, some people have oral microbiome imbalance, also known as dybsiosis.
Dysbiosis is a status where outgrowth of pathogenic bacteria leads to their accumulation, which results in inflammation. This inflammation is what makes your gums dark red and causes them to bleed.
How do I know if I have oral microbiome dysbiosis?
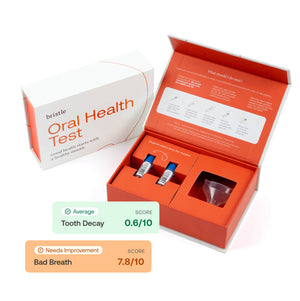
The gold standard to determine oral microbiome dysbiosis is through comprehensive oral microbiome testing, which can tell you what microbes are in your mouth and what you can do about it.
Some signs of oral microbiome dysbiosis are bleeding gums, tooth pain, gum redness, and persistent bad breath.
2. Improper flossing technique
Flossing should not cause bleeding gums! Routine flossing is critical to reducing accumulation of anaerobic periodontal pathogens at your gum line. Flossing removes food particles that can sit beneath the gums and feed pathogenic bacteria, and also removes biofilms, which serve as a home for pathogenic bacteria.
Flossing technique itself is important! We wrote an entire article about how to floss here, check it out! In short, flossing should not dig into the gums, but should curve around the base of the tooth between the gum and the tooth. You should stop when you feel resistance.
3. Oral thrush
Oral thrush is an infection, usually caused by a yeast called Candida. There are many species of Candida that cause thrush, but the most common one is Candida albicans. Thrush appears as white lesions, usually on the tongue, top of mouth, gums, or tonsils which are often painful to the touch and may give a burning sensation. Another symptom of oral thrush is persistent bad breath. Thrush is common in immunocompromised patients, such as people with HIV, and people on steroids or undergoing chemotherapy.
Oral thrush is another form of oral microbiome dysbiosis. Normally, the microbes in your mouth live in balance, keeping the abundance of the others in check. The oral microbiome is an ecosystem where each of its members interacts with others to maintain homeostasis. In the case of oral thrush, Candida are able to outcompete other microbes and grow to high abundance when they can cause oral thrush and bleeding gums.
4. Hormonal changes during pregnancy
It’s incredibly common for pregnant mothers to have what is known as pregnancy gingivitis. During pregnancy, changes in hormone levels can suppress your immune system, which allows periodontal pathogens to grow more rapidly. This bacterial growth leads to inflammation and increased bleeding. Additionally, pregnant mothers are more prone to swelling and bleeding because they are producing additional blood that helps the incubating baby grow.
You can reduce symptoms of pregnancy gingivitis by maintaining good oral hygiene, using effective antimicrobial mouthrinses to reduce the overall burden of pathogenic bacteria in the mouth. We recommend avoiding alcohol-based mouthwash as it generally has been shown to disrupt the healthy oral microbiome. Stabilized chlorine dioxide based mouthwashes are effective at reducing the abundance of anaerobic pathogens, and have some selectivity toward periodontal pathogens instead of the commensal oral microbiome.
Additionally, reducing plaque accumulation at the gum line can help reduce pregnancy gingivitis. A routine cleaning by a dental hygienist can remove this plaque and reduce symptoms of gingivitis.
5. Brushing too hard
Studies now show that using hard-bristled toothbrushes can cause gum abrasion, recession, and bleeding gums. 9 out of 10 dentists recommend that you use a soft-bristled toothbrush, and brush at a 45-degree angle to the gums.