In a recent episode of her podcast, Vitality Made Simple, renowned clinician Dr. Debbie Ozment, sits down with Bristle co-founder Danny Grannick, to shed light on a critically important yet often-overlooked pillar of our well-being - oral health. Their conversation sheds light on the power of proactive oral health practices, opening the door to a healthier, more vibrant life. It might just be that our smiles hold the key to a longer and more fulfilling life.
If you're intrigued by the idea of unlocking the secrets to longevity and better health through a holistic approach, you won't want to miss a minute of this insightful conversation.
Check out the full interview and explore the highlights below for more about the intersection of science, medicine, and the undeniable link between a healthy mouth and a healthier you
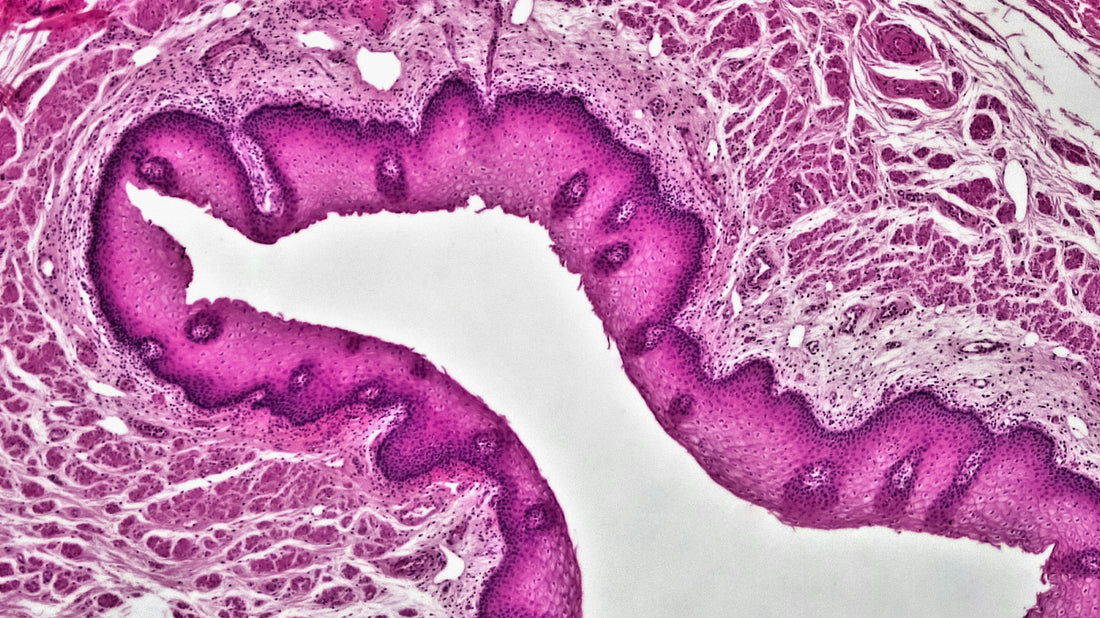
The Role of the Oral Microbiome in Oral Health and Disease
Dr. Debbie Ozment: The amazing thing about Bristle Health is that it really empowers you. You don't have to search for a dentist who is interested in balancing the oral microbiome. You can test yourself. This is so thrilling, Danny. So, what have you found in terms of diseases that the oral microbiome impacts?
Danny Grannick: We can split it up into two buckets. The first is the role of the oral microbiome in oral health and disease. The US Surgeon General actually put out a paper last year on oral health in America. Looking at the latest technologies, what the standard of care looks like.
He talks about the fact that the three most prominent oral diseases: periodontal disease, cavities (aka caries), and oral cancer all have an underlying microbial driver. The oral microbiome is really the foundation of oral health.
Then in the second bucket, you have this really interesting relationship between oral and overall health. Declining oral health has been correlated and associated with things like cognitive decline, increased risk of cardiovascular disease, or mismanaged diabetes. There is this biological underpinning where a lot of the pathogenic microbes in our mouths can migrate to other parts of our bodies and cause issues there as well. In about 2016, there was a paper that looked at patients with Alzheimer's and they were able to find P. Gingivalis, a keystone periodontal pathogen, in the brains of these patients. Since that landmark paper, there have been two therapeutics companies come to market targeting P. Gingivalis specifically, not to treat periodontal disease, but to slow the progression of Alzheimer's itself. The connection between our mouths and the rest of our bodies is very real.
Is the Oral Microbiome “Contagious”?
Dr. Debbie Ozment: A lot of these microbes are transmissible, “transkissible” I say. They're contagious. People can pass them on.
Danny Grannick: We do see a lot of similarities between partners living together. There have been a couple really exciting studies looking at parents and children that points to the child’s oral microbiome being seeded by the parents. We talk about nature versus nurture, right? And I think that that's especially true for oral health where there is obviously a nurture component where you make sure that you instill good behaviors and good practices. But there’s also a nature component where the predispositions or the oral microbiome imbalances in the parents can certainly have an influence and an effect on the child's oral microbiome and their future risk for oral conditions.
Dr. Debbie Ozment: Some people I see have type two diabetes and they'll say that it runs in the family. Well actually, what mostly runs in their family are habits, the foods they eat, activities they do. So, it's really similar to this. People are transferring their oral bugs to whoever they are kissing on or sharing a fork with. It’s really empowering for people to know.
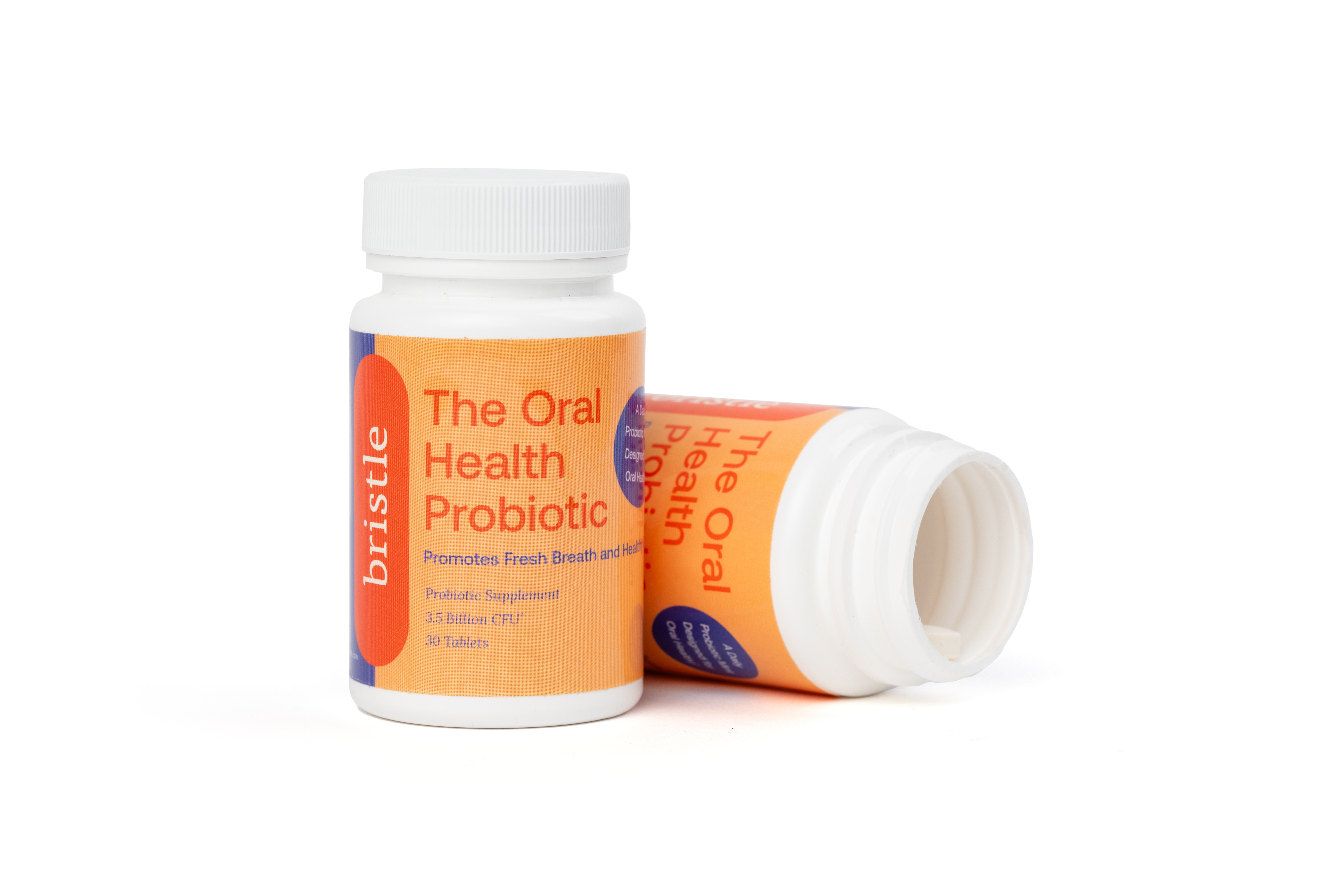
The Power of Early Detection and Preventive Care
Dr Debbie Ozment: In my practice, I see a lot of gut dysbiosis. I have learned that until we address it in the mouth, it will not be resolved in the gut. Even with antibiotics, it will go away and they'll feel better for maybe three months, but until the mouth is addressed, there won't be any real healing. It’s the root cause and if you're going to spend money on dentistry, this is basic. It's going to increase your dental implant outcomes to know what's going on in your mouth and to know exactly how to treat it.
Dentistry has progressed so much to be about cosmetics. What I've seen clinically is maybe they've had these beautiful veneers placed and they've spent $20,000, but they've got periodontal disease and their gums are shrinking away from the veneers and everything's potentially decaying.
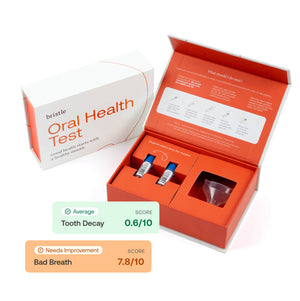
Danny Grannick: We see it a lot in other industries as well. The skin industry is full of a cosmetic-first approach and that's fine. Go try to get pearly white teeth, try to have fresh breath. And there’s nothing wrong with that. Just know that doesn't necessarily mean that you have good oral health. That’s why we always say test, don’t guess. So you know the actual health status of your mouth and can take action as needed.
Proactive Versus Reactive Medicine and Why It Matters
Danny Grannick: I think about reactive medicine in terms of when we detect and diagnose disease and what that means in terms of treatment. When we think about the typical dental visit, I go into the dentist and generally I'll receive an x-ray that looks for existing decay in my teeth and I'll receive an observational screening that looks for the physical presence and severity of symptoms in my mouth. That’s a very late-stage diagnosis. We're waiting until disease is manifested. Then your options are pretty limited in terms of what you can do to address it. It's going to be removing diseased tissue. It's going to be antibiotics and other relatively harsh, physical, expensive, and painful procedures.
In contrast a proactive or a preventive model is early detection of disease, really looking at the root cause agents and being able to predict risk. We’ve found the early signs of disease while it's still manageable and then can make fundamental changes to address it.
Dr Debbie Ozment: That is a very logical mindset, but a very rare mindset, unfortunately in our insurance driven system. We're not really trained to look preventively. This has to be a real grassroots effort. I think it has to be patient driven. When patients take the Bristle test results to their dentist and say ‘this matters to me’.
It's evident that our oral microbiome, a vibrant community of fungi, viruses, and bacteria, holds the key to unlocking a healthier future. As emphasized by Dr. Debbie and Danny, a simple saliva test can offer groundbreaking insights into our oral and overall health. This knowledge not only paves the way for personalized health strategies but empowers us to take control of our oral health journey. Let's seize this opportunity to foster a brighter, healthier tomorrow.