How many people do you know living with diabetes? Relatives (dead or alive), friends, coworkers? With 10% of Americans diagnosed with diabetes, you likely know someone. What about yourself? Do you know your own risk of developing diabetes?
In the United States, 34.2 million people of all ages are living with diabetes. Despite so many people with this diagnosis, many do not realize they have it until the disease is dangerously progressed [1].
Poor oral health is connected to diabetes. In a recent study, 18% of individuals with severe oral gum disease were unaware they already had diabetes. At the same time, people already diagnosed with diabetes are at greater risk of oral health problems and may not know to pay special attention to the health of their mouths [2].
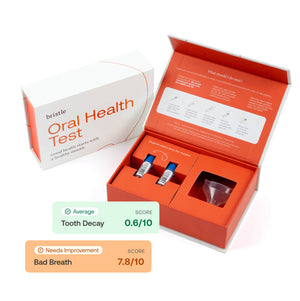
Once diagnosed, proper management of diabetes should encompass the many ways diabetes can impact health, including oral health. Recent studies have pointed to ways these two disorders are connected. More knowledge about your oral microbiome can help you to practice better prevention and care. Bristle’s oral microbiome test can give you more information about the state of your mouth.
Oral Microbiome & Oral Health
One way to evaluate oral health is by looking at the oral microbiome. Your oral microbiome is a unique set of up to 700 species of bacteria and other microbes that live in your mouth. The composition of your oral microbiome can both reveal and determine your oral and systemic health—influencing gum disease, other oral diseases, and diseases in the rest of your body, including diabetes.
What is Diabetes?
The name “diabetes'' means “passing too much urine” in Greek and was coined in the 2C AD [3]. Diabetes is a disorder that impacts how your body processes the food it takes in. Typically, when you eat carbohydrates (fats and proteins are handled differently), secretions in your saliva, stomach and small intestine break them down into glucose, a simple sugar that your blood carries to feed all your cells and tissues.
When that sugar hits the bloodstream and raises your blood glucose level, your pancreas notices, and releases insulin. The insulin then signals to your cells to take up that glucose and turn it into energy [4].

https://medmovie.com/library_id/3255/topic/ahaw_0249i/
However, when you have diabetes, your pancreas either does not release enough insulin (all type 1 diabetics and some type 2) or cells in your muscles, fat, and liver become insulin resistant (most type 2 and gestational diabetes cases). If enough glucose builds up in the blood, it produces adverse health effects like frequent urination and unintended weight loss, eventually serious illness, even permanent damage to the eyes, kidneys, nerves, and other tissues.
There are three widely accepted types of diabetes: type 1, type 2, and gestational [5]. Some researchers have suggested additional types and subtypes, including one related to dementia.
Type 1:
Type 1 diabetes is when your pancreas stops making insulin. Researchers believe this is due to an autoimmune reaction that kills the pancreatic cells (Islets of Langherans) that make insulin.
Only 5-10% of people with diabetes have type 1. It is typically diagnosed in children, teens, and more rarely, adults. Patients must replace their missing insulin every day to survive.
Type 2:
Type 2 diabetes is different because, in this case, the pancreas does produce insulin. But certain tissues: fat, muscle and liver cells, do not respond to the insulin signal (insulin resistance). Around 90-95% of people with diabetes in the US have type 2.
Most often, type 2 diabetes adults are classified as overweight or obese, making up around 89% of all diabetic cases. However, type 2 diabetes can occur in people with normal BMIs. In part related to increasing obesity, children, teens, and young adults are increasingly likely to be diagnosed with type 2 diabetes.
Gestational diabetes
This type of diabetes occurs during pregnancy. For most mothers, the diabetes disappears after the baby is born. However, gestational diabetes means the woman has a greater chance of developing type 2 diabetes later in life.
How does oral health relate to diabetes?
The relationship between oral health and diabetes is what scientists call bidirectional, meaning that both diseases influence one another. The specifics of this relationship include disease prevalence, risk factors, prevention, and treatment. It is important to look at this relationship to better understand how these two diseases affect each other for better prevention, treatment, and management [6].
High prevalence of diabetes and gingivitis
One reason scientists are interested in both of these diseases and the ways they connect is because of how prevalent both diseases are in the US. Most adults suffer from some type of periodontal disease, with around 90% of the population suffering from gingivitis (mild-moderate gum disease). Within that group of adults, for those over 30, 50% of them suffer from periodontitis, a more severe gum disease that breaks down soft and hard tissues that surround teeth [7].
Diabetes is also highly prevalent, and prevalence is growing rapidly, making it a major health concern. Diabetes is present in about 13% of the adult population in the United States, meaning around 34.1million people.
Who is at risk for diabetes and gum disease?
Many risk factors for type 2 diabetes and gum disease overlap, thus managing these risk factors can improve outcomes for both diseases.
Family history/genetics
These are important, but out of your control. Nevertheless, knowing that near relatives have had diabetes should alert you that you are at higher risk. If family history matters, we know there are genetic patterns associated with diabetes and poor oral health. DNA tests can help you find out if you have genetic patterns that increase your risk of diabetes.
Smoking
Smoking increases your risk of getting diabetes, as nicotine produces insulin resistance [9]. Smokers are 30-40% more likely to develop diabetes than non-smokers. At the same time, smoking can also increase your risk of developing gum disease [10]. Quitting smoking is one way to target both diabetes and gum disease prevention and control [11].
Obesity
Obesity is a top risk factor for type 2 diabetes (~90% of type 2 diabetics are overweight or obese) [12,13], and can also put you at risk of gum disease [14]. Choices like good nutrition (limiting sugar) and physical activity can both help control your weight and reduce your risk of diabetes and obesity. You may also want to consider your body mass index (BMI, a measure of fat index in the body) and how to stay within healthy BMI ranges.
Inflammation
Inflammation is a key issue in both diabetes and gum disease. Acute inflammation is a natural response in the body to attacks by pathogens, but when inflammation stays too high over time, it becomes chronic. Chronic inflammation seems to be a contributing factor to multiple diseases like cancer, autoimmune diseases, arthritis, heart disease and, in this case, diabetes and gum disease [15].
Onset: Early signs of type 2 diabetes and gum disease
Given that both of these diseases are so prevalent, knowing what to look out for as warning signs of disease can help you get treatment faster.
Early symptoms of type 2 diabetes
You might have type 2 diabetes if you have symptoms like:
Early signs and symptoms of gum disease
Some signs of gum disease include:
Does gum disease cause type 2 diabetes or vice versa?
As we mentioned, there is an established bidirectional relationship between type 2 diabetes and gum disease, but whether they cause each other or one always comes first has not been determined.
The best research can only tell us about the strong correlations and the similar risk factors. Most studies are limited to examining the microbiomes of people already diagnosed with diabetes. This means we don’t have enough information comparing the microbiome over time in people who go on to develop diabetes.
One study found that a different mix of bacterial species are more likely to be found in the oral microbiome of those with type 2 diabetes. It’s unclear how these specific patterns of dysbiosis cause diabetes. However, it does suggest that the oral microbiome may influence the development of diabetes or that diabetes influences the oral microbial ecosystem [16]. This is another reason to participate in oral microbiome testing and studies, to help build a database that will help answer these questions.
Type 1 Diabetes & Oral Health
Although we’ve focused on type 2, there is a relationship and impact between type 1 diabetes and oral health [17]. People with type 1 diabetes are also at greater risk of developing gum disease. Moreover, type 1 diabetes patients are more likely to have poorer overall dental health. Specifically in children, research has found that they are also more likely to have gum disease and plaque build-up [18].
Here’s one way that diabetes may cause gum disease. Diabetes can elevate oral inflammation, increase sugar levels in saliva and encourage bacteria to grow. These bacteria can then impact the oral microbiome and lead to gum destruction. Elevated levels of bacteria were found in those with type 1 diabetes.
Even more, people with poorly controlled diabetes, for example, those having to go to the emergency room, were even more likely to have gum disease, which suggests that poor diabetes management contributes to gum disease. Although it should also be noted that those experiencing poverty, mental illness, lack of education and other hazard factors may have poorer oral hygiene in general as well [19].
Type 2 Diabetes & Oral Health
Given the bidirectional relationship between type 2 diabetes and gum disease, it should come as no surprise to you that oral health and habits shape some of this relationship. Research has found multiple oral bacteria to be associated with diabetes, and suggests that the oral microbiome may be important to the development of diabetes [20].
On the other hand, some researchers are more concerned about the general lack of knowledge from the public, those that have diabetes, and the medical community, on ways to combat both diseases. They argue that physicians should be educated about oral disease and diabetes to help combat oral disease earlier on. It also calls for further research on the relationship and how health disparities impact both. They argue that the lack of knowledge and access to health and oral care needs to be addressed to ultimately determine the relationship [21].
Gestational Diabetes & Oral Health
Gestational diabetes has also been shown to have an impact on women’s oral health, and potentially vice versa. In fact, in one study run by the College of Dentistry at NYU, they found that women with gestational diabetes had higher levels of gum bacteria and general inflammation. Such studies highlight the importance of women going to the dentist before, during, and after pregnancy as well as practicing consistent dental hygiene [22].
Some scientists point to general inflammation during pregnancy to be reason for concern, and something that dentists and health care professionals should be aware of when women are pregnant and have gestational diabetes, to avoid making these conditions worse [23].
How does diabetes affect oral health?
In addition to understanding how diabetes might influence oral health, we should also look at how diabetes might influence oral disease.
Periodontal disease
Diabetes may make periodontal disease (that is, gum disease) more severe, as it intensifies inflammation and makes gum healing more difficult. With more severe gum disease, it makes metabolism and glycemic control more difficult, which may worsen diabetes [24].
Oral disease
Diabetes also is associated with several oral diseases, such as taste impairments, mouth ulcers, oral fungal infections (thrush), and more. Saliva dysfunction and an unhealthy oral microbiome can worsen certain oral conditions [25].
Lessons from Diabetes & Oral Health
Given how intertwined these two diseases can be and the adverse effects both have on the rest of the body, dental care and dental health are key. Researchers suggest more communication between medical care teams and mutual referrals between PCPs, endocrinologists and dentists in managing diabetes. This can help patients better understand both diseases and take steps to mitigate each, to ultimately improve management of both diseases [26].
Educate yourself about diabetes and oral health
Since diabetes and oral disease are so prevalent in the United States, and since both are easily overlooked in their early stages, it’s a good idea to educate yourself. Of course, reading materials such as this can help you learn, but other ways you can support yourself include:
Knowing your Diabetes Risk
Part of educating yourself about diabetes is evaluating your risk factors for diabetes and seeing whether a diabetes test is prudent.
Type 1 Diabetes Risk
Risk factors include family history, so if anyone in your family has type 1 diabetes, you are more likely to be diagnosed as a child, young adult or teen.
Type 2 Diabetes Risk
The risk factors for type 2 diabetes include family history and age as well (incidence of diabetes increases at 45 years or older). However, other risk factors include
Additionally, African American, Hispanic/Latino and American Indians or Alaska Natives are at greater risk.
Gestational Diabetes Risk
Gestational diabetes risk is similar to type 2 risk factors, however it also includes factors like:
Prediabetes Risk
Prediabetes risks are the same as type 2 diabetes risk factors. Prediabetes can be avoided or delayed by eating healthy, exercising and maintaining a healthy weight.
If you are at risk of diabetes, you may want to consider a diabetes test. Diabetes tests typically include blood tests to evaluate your blood sugar levels. The main tests to measure this include an A1C test (evaluating your average blood sugar over time), a fasting blood sugar test, and a glucose tolerance test. You may want to consider annual blood tests if you are at risk of diabetes [28].
Know your oral health risk
Talk with your dentist about risk factors: Starting an open, honest conversation with your doctor and dentist about risk factors can help you understand your own risk better and make lifestyle changes to keep you healthy.
Dental hygiene: self-care and dentist visits
One of the best ways to keep good care of your oral health is by implementing a solid hygiene routine at home and making a regular dental visit [29].
Simple habits like brushing and flossing daily can go a long way. Regular, professional dental cleaning can not only remove plaque and tartar that escaped your daily care, it can also help keep you informed on your gum and tooth health.
How Bristle can help you keep tabs on your oral health
Bristle analyzes the oral microbiome to assess your oral health status, and show you risk factors for tooth decay, gum disease, and bad breath. We then help you determine what’s working in your oral care routine and what’s not and make personal recommendations based on your own personalized oral health insights to keep your mouth healthy. Interested in learning more? Get your kit today!
Citations:
1. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pd
2. https://drc.bmj.com/content/5/1/e000326
3. http://www.hormones.gr/760/article/article.html
4. https://open.oregonstate.education/aandp/chapter/23-7-chemical-digestion-and-absorption-a-closer-look/
5. https://www.cdc.gov/diabetes/basics/diabetes.html
6. https://www.sciencedirect.com/science/article/abs/pii/S0002817714638836
7. https://pubmed.ncbi.nlm.nih.gov/33651538/
8. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
9. https://synapse.koreamed.org/articles/1084624
10. https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/pdfs/fs_smoking_diabetes_508.pdf
11. https://synapse.koreamed.org/articles/1084624
13. https://www.niddk.nih.gov/health-information/diabetes/overview/risk-factors-type-2-diabetes
14. https://www.scielo.br/j/csc/a/Zf58WTKZXQxg5h6XsLzLGbT/?lang=en
15. https://www.health.harvard.edu/staying-healthy/understanding-acute-and-chronic-inflammation
16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5403709/
17. https://www.sciencedirect.com/science/article/pii/S0929664618305941
18. https://www.degruyter.com/document/doi/10.1515/jpem-2017-0053/html
20. https://onlinelibrary.wiley.com/doi/abs/10.1111/jre.12432
21. https://www.sciencedirect.com/science/article/abs/pii/S000296291530687X
22. https://www.sciencedaily.com/releases/2008/03/080324122301.htm
24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3623289/
25. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3623289/
26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8257029/
27. https://www.diabetes.org/a1c/diagnosis
28. https://www.cdc.gov/diabetes/basics/getting-tested.html
29. https://www.dentistryiq.com/dental-hygiene/clinical-hygiene/article/16359771/screening-for-diabetes-in-the-dental-office