Did you know that bad breath can be caused by dozens of different types of microbes in the mouth? Halitosis does not have a single cause, and is a consequence of the diverse set of microbes in the oral cavity.
Chronic bad breath is generally caused by microbial imbalance in the mouth, which can lead to the outgrowth of many different kinds of microbes that cause bad breath, like Solobacterium moorei, Tannerella forsythia, Candida albicans, Porphyromonas gingivalis, and many more. In this article we go over each of the types of bacteria that cause bad breath, where they live, and finally how this data can help you solve your chronic halitosis.
Where does bad breath come from?
There are different types of halitosis, which can be grouped by the microbes that cause it, and the locations where they typically grow. Each type of bad breath can be addressed with specific evidence-based regimens that tackle oral microbiome dysbiosis at its root, leading to a more stable microbiome that can prevent bad breath.
90% of bad breath comes from the mouth, but the mouth has dozens of niches where microbes can grow and cause bad breath. Halitosis from the mouth is caused by oral microbiome dysbiosis, the imbalance of microbes in the mouth that leads to outgrowth of species that cause disease. Normally, in healthy people, the oral microbiome has low levels of bacteria that can cause bad breath.
These odor-producing bacteria are an important part of your oral microbiome, because they can help train your immune system or make molecules that are important for health. For example, low levels of hydrogen sulfide are beneficial in reducing inflammation. However, higher concentrations of hydrogen sulfide can cause tissue damage and worsen gum disease, in addition to causing bad breath.
Different types of halitosis
So far, Bristle’s comprehensive oral microbiome test has identified bad breath in the following types:
- Inflammatory gum bacteria
- Non-inflammatory gum bacteria
- Opportunistic Enterobacteriaceae
- Tongue coaters
- Fungal
- Intermittent bad breath
Each of these types will respond better to some oral health regimens than others. Traditional hygiene routines of brushing and flossing are also not sufficient to fix all types of oral microbiome dysbiosis.
In this article we won't discuss bad breath from the gut, as research shows less than 10% of bad breath comes from the gut. But watch for future articles about bad breath from the gut, and what you can do about it!
Inflammatory gum pathogens cause bad breath
These are pathogens that live at your gum line and cause gum disease that can also cause bad breath. Some of these pathogens can also be found in the crypts of the tongue, which can be a reservoir for these bacteria. A few examples of the species that contribute to this type of bad breath are:
- Porphyromonas gingivalis
- Treponema denticola
- Tannerella forsythia
- Prevotella nigrescens
- Fusobacterium nucleatum
- Prevotella intermedia
- Eubacterium brachy
- Porphyromonas endodontalis
This is the most common type of bad breath. Anaerobic bacteria (ones that can only grow in the absence of oxygen) live at or beneath the gum line (also known as subgingival plaque), where they ferment food, debris, protein, and sugar in your saliva. They can even metabolize cellular debris as they cause damage to the cells that line your gums. In people with severe oral microbiome dysbiosis, these anaerobic pathogens can grow to high levels and cause gum disease.
These bacteria can be difficult to remove for people with gum disease, as gum recession and inflammation makes it challenging to clean deep within gum pockets. Additionally, inflammatory gum pathogens can silently accumulate over time, causing persistent bad breath without any other symptoms of gum disease such as bleeding or tender gums.
Non-inflammatory gum bacteria can cause bad breath
These are bacteria that live at the gumline or on the tooth surface and don’t typically cause inflammation, yet can cause bad breath.
- Selenomonas noxia
- Selenemonas artemidis
- Dialister invisus
- Eikenella corrodens
- Leptotrichia wadei
These bacteria typically take advantage of plaque that accumulates on your teeth or at the gum line (subgingival and supragingival plaque). The plaque provides a stable environment for these microbes to continuously grow back, even after brushing, flossing, or using mouthwash. Some of these microbes can survive in both the presence and absence of oxygen, but often grow best in anaerobic environments.
Tongue coaters can cause bad breath
Tongue-coating pathogens live on the dorsum of the tongue, way in the back where oxygen is at its lowest. The grooves and niches of your tongue can harbor biofilm that is hard to reach. Here are some bacteria on the dorsum of the tongue that cause bad breath:
- Atopobium parvulum
- Solobacterium moorei
- Eikenella corrodens
- Leptotrichia wadei
- Peptostreptococcus stomatis
- Prevotella shahii
These bacteria live in the pits on top of the tongue, also known as lingual papillae. These pits and crypts give the tongue its rough texture, and also allow for a dynamic community of microbes to thrive. The microbes that live in these crypts can cause inflammation, leading to inflammation in the crypts, which is a main cause of white tongue coating.
While the coating itself can be scraped away, the microbial community remains in the crypts, can rapidly grow back, and is often associated with chronic bad breath. Sometimes white coating can appear and disappear spontaneously, which can also cause intermittent bad breath (covered more in depth later in this article).
Other conditions, such as oral thrush or leukoplakia, can also cause tongue coating.
Opportunistic Enterobacteriaceae can cause bad breath
Enterobacteriaceae is a family of bacteria, which includes species you may have heard of, such as Escherichia coli, Klebsiella pneumoniae, and Enterobacter faecalis. This microbes are commonly found in both the gut and the mouth, and can grow in both aerobic and anaerobic conditions. These are also opportunistic pathogens, meaning in some cases they can cause infections and take over a community. In many cases, it’s not clear where they colonize, though some studies suggest that a reservoir of Enterobacteriaceae may come from the tonsils. People with this type of bad breath typically have lower diversity in their oral microbiome and are dominated by any of the following species:
- Enterobacter cloacae
- Enterobacter aerogenes
- Enterobacter faecalis
- Klebsiella pneumoniae
- Klebsiella oxytoca
These pathogens can be highly drug resistant, and are a major cause of hospital-acquired infections. They often appear suddenly after a dose of antibiotics. They have also been shown to persist in the oral cavity, through periods of starvation, making them notoriously challenging to tackle. Additionally, these bacteria can colonize a variety of places, including the sinuses, tonsils, and gums. Oral microbiome dysbiosis with high levels of these bacteria may require more extensive treatment to fix.
Fungal causes of bad breath
An overabundance of Candida, the cause of oral thrush, can cause bad breath. Here are species to look out for:
- Candida albicans
- Candida tropicalis
- Candida dubliniensis
- Candida glabrata
Fungi like Candida normally live at low abundance in the oral microbiome relative to bacteria. Under healthy conditions, Candida can help prevent infection by other microbial pathogens. However, microbiome dysbiosis can cause Candida outgrowth, leading to invasive Candida infection, also known as Candidiasis or oral thrush. Oral thrush can present as whitish yellow lesions on the tongue, cheeks, and gums. People who smoke and immunosuppressed patients are often susceptible to Candidiasis. Fortunately, prescription anti-fungals are effective at treating Candida.
Intermittent bad breath
This is the most challenging and diverse type of chronic halitosis. Many people suffer from persistent, yet intermittent bad breath. Some days after their oral hygiene routine, they experience fresh breath, and other times bad breath is more severe.
The cause of this intermittent bad breath is likely a mix of the oral microbiome, diet, and lifestyle. Microbes compete for space and nutrients in the oral cavity. Food particles, metabolites in saliva, and hygiene changes can trigger dramatic shifts in the community. We don’t yet fully understand the complex dynamics of these shifts, but research is beginning to reveal how specific bacteria can prevent outgrowth of foul smelling microbes that cause bad breath, and specific diet, lifestyle, and hygiene routines can boost those specific beneficial bacteria.
People with intermittent bad breath may have the following:
- Extremely low microbiome diversity.
- Atypical species in the oral microbiome.
- At Bristle, fewer than 1% of all samples have “completely unexpected” results with unusual species in the microbiome.
- Multiple sources of bad breath bacteria on the tongue, gums, and teeth.
- Higher variation in their microbiome from day to day
Treating bad breath
While most of us have tried various ways to mask bad breath like gums and mints, these are all temporarily solutions. In order to eliminate bad breath, we need to shift the oral microbiome to a state of balance.
To do so, there are a number of different tools you can use like eating or avoiding certain foods and using certain types of oral care products in your hygiene routine. However, just like not all bad breath is the same, not every combination of solutions will work for all individuals. Based on the type of bad breath, there are different solutions that will work better than others and require the proper timing & usage to be truly effective.
So how can you fix each of these types?
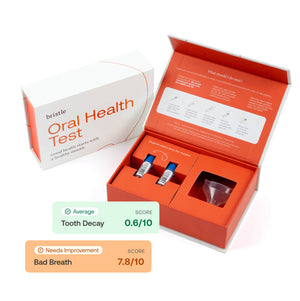
- Get the data! There’s no reason to go about this blindly. Oral microbiome testing can guide data-driven decisions about your own health, including how to fix persistent bad breath.
- Use science! Decades of microbiology research have revealed methods to reduce specific microbes, but it’s important to know which bacteria are there to guide the most effective treatment. At Bristle, we use our own internal database and clinically demonstrated methods to improve the oral microbiome. Given your health history and microbiome data, our oral health coaches will build a care plan with you to help treat, manage and prevent disease.